Addressing Mental and Physical Health in Vulnerable Patients During the COVID-19 Pandemic
RELEASE DATE
May 1, 2021
EXPIRATION DATE
May 31, 2023
FACULTY
Tammie Lee Demler, BS, PharmD, MBA, BCGP, BCPP
Clinical Associate Professor
State University of New York at Buffalo School of Medicine
Department of Psychiatry
Director of Psychiatric Pharmacy Residency Programs
State University of New York at Buffalo School of Pharmacy and
Pharmaceutical Sciences
Buffalo, New York
FACULTY DISCLOSURE STATEMENTS
Dr. Demler has no actual or potential conflicts of interest in relation to this activity.
Postgraduate Healthcare Education, LLC does not view the existence of relationships as an implication of bias or that the value of the material is decreased. The content of the activity was planned to be balanced, objective, and scientifically rigorous. Occasionally, authors may express opinions that represent their own viewpoint. Conclusions drawn by participants should be derived from objective analysis of scientific data.
ACCREDITATION STATEMENT
 Pharmacy
Pharmacy
Postgraduate Healthcare Education, LLC is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education.
UAN: 0430-0000-21-055-H01-P
Credits: 2.0 hours (0.20 ceu)
Type of Activity: Knowledge
TARGET AUDIENCE
This accredited activity is targeted to pharmacists. Estimated time to complete this activity is 120 minutes.
Exam processing and other inquiries to:
CE Customer Service: (800) 825-4696 or cecustomerservice@powerpak.com
DISCLAIMER:
Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patients’ conditions and possible contraindications or dangers in use, review of any applicable manufacturer’s product information, and comparison with recommendations of other authorities.
GOAL
To identify the factors associated with SARS-CoV-2 that have exacerbated a parallel mental-health crisis among vulnerable patient populations during the COVID-19 pandemic, and address vaccine hesitancy as a means to improve community mental health and safety and increase the likelihood of developing herd immunity.
OBJECTIVES
After completing this activity, the participant should be able to:
- Recognize the impact of the COVID-19 pandemic on mental health in the community.
- Identify health disparities experienced by individuals with mental illness that may predispose them to SARS-CoV-2 infections.
- Describe opportunities for pharmacy personnel to participate as members of the COVID-19 response team.
- Discuss the educational opportunities available to address vaccine hesitancy during the ongoing pandemic.
ABSTRACT: The COVID-19 pandemic has resulted not only in physical illness and death but it has also precipitated an evolving mental-health crisis. The importance of widespread vaccination is accepted as the best medical hope to lead us out of the pandemic, but that will require population herd immunity to ensure that most people can be considered protected. Addressing vaccination hesitancy, especially that associated with the COVID-19 vaccine, is challenging and can be made even more so by health disparities experienced by individuals in vulnerable groups, including those with mental-health disorders. These disparities may also predispose patients to greater risk of SARS-CoV-2 infection and associated complications. To provide optimal care for patients diagnosed with mental-health disorders and those who have other predisposing disparities during the COVID-19 pandemic, pharmacists should have a comprehensive understanding of how these clinical factors may uniquely impact this population and identify and take advantage of opportunities to address them.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is responsible for causing the current coronavirus disease 2019 (COVID-19) pandemic that has plagued the world for more than a year. Forced changes to normal human behavioral patterns leading to isolation and restricted activities secondary to mandated quarantines are predicted to increase exacerbations of current psychiatric disorders as well as to contribute to newly emerging conditions.1 With vaccination distribution staged such that the most susceptible were prioritized to receive the limited supplies of vaccine available, there is palpable anxiety in those still waiting for their turn to become vaccinated. And despite the reported safety and efficacy of the vaccines currently available, there continue to be individuals who are vaccine hesitant and those who strongly oppose accepting the COVID-19 vaccine. With studies reporting that nearly half of patients with confirmed SARS-CoV-2 infection do not exhibit symptoms, the hesitant may be even less inclined to vaccinate. However, in the scientific community, there are significant concerns about both the short- and long-term side effects of contracting the COVID-19 infection, both in those who did not show evidence of illness and those who experienced a severe infection.2-4
Impact of COVID-19 on Mental Health
While the milder physical symptoms of COVID-19 infection are now well known, with hallmark symptoms including cough, fever, loss of taste and smell, and gastrointestinal symptoms, for some, these symptoms continue to spiral into a more severe illness including acute respiratory distress syndrome, organ failure, and death.2,5 Less frequently considered is the substantial occurrence of notable neurologic side effects associated with COVID-19 and psychiatric consequences that can be particularly worrisome for individuals with, for example, pre-existing psychotic disorders.6 Research is underway to evaluate the potential association of morbidity and mortality for those who develop neurologic symptoms and conditions after COVID-19 infection and whether these individuals might be at a greater disadvantage than their infected counterparts who experience only the physical symptoms of infection.6
The induction of mania, psychosis, depression, and anxiety, among other psychiatric symptoms, has been reported in those who have been infected by the virus.7-10 Underlying mental illness is also thought to be responsible for eliciting a more intense emotional response as a result of the COVID-19 epidemic, resulting in relapses, or worsening, of an already existing mental-health condition because of greater susceptibility to stress compared with the general population.11 Governmental travel restrictions and quarantine orders have also been reported to have disproportionately affected individuals with mental-health disorders who need regular outpatient visits for evaluations, for administration of long-acting injections, and for medication-management and refills.11
Pediatric Patients: Pediatric patients have also experienced a significant impact, with the Centers for Medicare & Medicaid Services (CMS) reporting 44% fewer outpatient mental-health services between March and May 2020 than in that period the previous calendar year, even after accounting for increased telehealth services during the first few months of the pandemic.12 The CDC reported a 24% increase in emergency mental-health visits in children aged 5 to 11 years and an even greater increase, 31%, for older children and adolescents aged 12 to 17 years between April and October 2020.13 Researchers are exploring whether increased susceptibility to stress and mental-health disorders may be precipitated by the virus itself.14-16 A shared belief among experts in the field is that the COVID-19 pandemic has precipitated a parallel epidemic of fear, depression, and anxiety.11
Older Adults: As for the impact of the pandemic in older adults, it has been recognized that the isolation caused by stay-at-home orders has been especially difficult for the geriatric population and people with preexisting mental illness.17 Food insecurity, isolation, and the economic instability associated with COVID-19 is adding to the baseline stress that underserved populations experienced prior to the pandemic. Additionally, the public-health actions recommended to reduce the spread of infection, including social distancing and quarantine, may precipitate anxiety and depression in anyone predisposed to effects of pandemic stress, especially those with pre-existing mental-health conditions, in the community.18
Cognitively Impaired Adults: Individuals with cognitive impairment may experience altered awareness of their risk of infection and may not make the appropriate accommodations to prevent infection, such as using personal protection (e.g., masks and hand sanitizer). They may make diminished efforts to ensure appropriate social distance, especially in congested living spaces they may share or socialize within, and often face more barriers to accessing health services in a timely way.11 Therefore, pharmacists should seize every opportunity to educate individuals who may experience cognitive impairment, such as older adults and individuals with neurologic or psychiatric illness, on opportunities to reduce their personal risk of infection. Ptacek and colleagues write that the importance of maintaining mental health during this viral pandemic will have significant societal impacts not only on the COVID-19 survivors but also on achieving the goal of establishing functional herd immunity overall. Thus, the pharmacist’s role in educating these at-risk populations takes on a more global importance when advocating for increased support and research in this specific population.1
Healthcare Workers: Another vital segment of our community that has been impacted by COVID both physically and mentally is healthcare workers serving on the frontlines, who are not only experiencing the parallel pandemic of anxiety and fear but also the stress and strong emotions associated with caring for the sick and dying. This situation requires heightened vigilance to monitor for personal well-being. According to the CDC, “compassion fatigue” has taken its toll and has contributed to the already existent burnout that those caring for others at work and at home encounter.19 Many adults have reported negative impact on well-being and mental health, with sleep disorders (36%) or changes to eating patterns (32%) and increases in alcohol consumption or substance use (12%) reported due to worry and stress over the coronavirus.20
COVID-19 Survivors: COVID-19 survivors, including those with pre-existing mental-health conditions, may have an elevated risk of suicide, and these rates are expected to continue to increase and may even peak after the actual pandemic ends. Efforts to minimize stress, fear, anxiety, and loneliness have been recommended as focused strategies to reduce suicide rates during the COVID-19 crisis.21
Health Disparities, Mental Illness, and COVID-19
The COVID-19 pandemic is having a significantly negative impact fiscally, mentally, and medically on patients with chronic disease. Nemani and colleagues explored whether individuals diagnosed with schizophrenia-spectrum disorder, anxiety disorders, and/or mood disorders were associated with higher mortality rates among patients diagnosed with COVID-19.22 Prior to their research, the association of psychiatric diagnoses with mortality in patients had not been specifically evaluated and reported. The retrospective study assessed 7,348 adult patients for 45 days after their diagnosis with laboratory-confirmed COVID-19 infection and measured mortality, defined as discharge to hospice or death within that same period of time. Of the patients meeting the inclusion criteria with positive test results, 7.7% (564) had a history of a mood disorder, 4.9% (360) had a history of an anxiety disorder, and 1% (75) had a history of a schizophrenia-spectrum illness. Once demographic- and medical-risk factors such as hypertension, diabetes, cancer, chronic obstructive pulmonary disease, and positive smoking status, among other factors, were adjusted for, the authors reported that individuals with a diagnosis of a schizophrenia-spectrum disorder had more than twice the risk of mortality from COVID-19 when compared with their peers without a psychiatric disorder (odds ratio [OR], 2.67; 95% CI, 1.48-4.80).22
Individuals without a diagnosis of schizophrenia but who had hypertension or diabetes or were current smokers were also at increased risk of COVID-related death, but not to the same degree as those diagnosed with schizophrenia-spectrum illness. However, individuals with diagnoses of anxiety or mood disorders were not observed to experience this same disproportionate COVID-related mortality (OR, 0.96; 95% CI, 0.65-1.41 and OR, 1.14; 95% CI, 0.87-1.49, respectively). Not surprisingly, additional factors that increased the risk of COVID-related mortality included being male, having heart failure, and/or being a race other than white. Older age (age 45 years or older) was also a risk factor.22 Researchers hypothesize that individuals with schizophrenia may have an altered immune response to infection, with some studies suggesting that severe infections may precede the diagnosis of schizophrenia. Therefore, the susceptibility to COVID-19 of individuals with serious mental illness (SMI) may be a consequence of both the adverse cardiovascular impact of psychiatric medications and altered immunity; this requires further study.22
Role of Racial and Ethnic Disparities
Racial and ethnic disparities have been noted as “red-flag” alerts to the physical health vulnerabilities of this additional at-risk population which is also disproportionately impacted by mental illness that may be worsened or caused by pandemic stress. To ensure that pharmacists provide optimal care to patients experiencing health disparities who are also comorbidly challenged by mental illness, these disparities must first be recognized.
The CDC highlights five fundamental areas that contribute to the disproportionate adverse effect of COVID19 on ethnic and racial minority groups, termed the social determinants of health.23 Although all five areas contribute to this disparity, there are some key areas where pharmacists may provide a uniquely beneficial impact when faced with managing individuals within these at-risk populations during this pandemic and beyond.
Access: The lack of access to healthcare may be due to either the absolute lack, or sheer inadequacy, of the availability of culturally or linguistically responsive healthcare. Additionally, individuals from ethnic and racial minority groups may lack trust in the healthcare system because of actual treatment or perceived inequity. This barrier increases not only the risk of poor health outcomes from inadequately managed underlying medical and psychiatric conditions but also more limited access to vaccination and treatment for COVID-19 infection.23 Pharmacists are considered to be among the most accessible healthcare professionals and are often available 24 hours per day, 7 days per week and, hence, can play an important role in increasing the availability of culturally and linguistically responsive healthcare and in reducing the mistrust experienced by some members of ethnic and racial minority groups.
Neighborhood and Physical Environment: A patient’s neighborhood and physical environment may contribute further to lack of healthcare access by creating barriers to reliable transportation to pharmacies and medical clinics. Another COVID consideration is that multiple generations of family members within these at-risk populations may live in one shared household, further increasing the risk of exposure and infection, especially in older adults living in this setting.23 For patients with SMI, overcrowding may result from necessary shared-housing solutions for those experiencing homelessness and abandonment. Pharmacies often provide delivery service, so this factor should play a role in the medication-management considerations for patients with limited or absent mobility.
Education and Lower Literacy: People from racial and ethnic minority groups are disproportionately more likely to experience lower literacy, decreased high school–completion rates, and other barriers to college admission.23 This literacy gap extends to individuals with SMI, and it has been suggested that health literacy improvements may have great potential to impact health outcomes for this typically underserved population.24 Health literacy is defined as the degree to which individuals have the capacity to obtain, process, and understand basic health information and the services needed to make appropriate health decisions.25
Chronic disease prevention and management, including that necessary with psychiatric conditions, requires a minimum threshold of health literacy in order to read, comprehend, and make decisions based on communication with healthcare providers.24 Individuals with SMI have been reported to have lower health-literacy rates due to not only lower socioeconomic status but also the functional and cognitive impairments that may accompany the presence of a mental illness.24,26,27 Clausen and colleagues reported that when compared with national health assessments that measure approximately 26% of adults in the general population as having basic or below-basic health literacy levels, the prevalence of similarly inadequate literacy for peers with SMI is nearly double that.24 Pharmacists should be constantly aware of this potential void and make accommodations whenever there is a suspected gap of understanding and comprehension.
Income and Wealth Disparity: The income and wealth disparity associated with lower incomes, larger debt, and unsuccessful efforts to accumulate wealth can result in individuals facing complications in managing expenses, challenges with paying medical bills, and difficulties with access to healthy food. According to a survey conducted in June 2020, of the 5,000 respondents with diabetes, 25% reported having to borrow money, using savings or stimulus money, or rationing prescribed insulin by modifying dose or frequency of use. This same survey revealed that roughly 50% of those in the lowest income brackets lost most, or all, of their income and that unemployment was associated with discontinuation of prescription and medical insurance coverage.28,29 Individuals with SMI are at increased risk of metabolic syndrome, which is a cluster of recognized cardiovascular risk factors that in addition to hyperglycemia and diabetes also includes dyslipidemia, abdominal obesity, and hypertension. In addition to the contribution of antipsychotic medication to metabolic syndrome, this predisposition is thought to also be due, in part, to unhealthy lifestyle choices and a poor adherence to a recommended medical regimen.30
Occupation and Job Conditions: Essential workers, such as those in healthcare, transportation, and food processing and production, have a greater chance of exposure to COVID-19 because their jobs involve close contact with the public and fellow workers. These workers, who often experience racial and ethnic disparities in addition to these high-risk job conditions, may also lack the paid sick days needed if they contract COVID-19.
According to the CDC, to slow and eventually stop the spread of COVID-19, the community needs to ensure equity in the availability of resources to maintain physical and mental health; these resources include access to affordable testing as well as physical and mental healthcare that meet the needs of the individuals comprising these diverse communities. Resources include easy access to information, goods, and services, affordable testing, and medical and mental healthcare that is tailored to meet the needs of people from diverse communities.23
Pharmacists’ Role on the COVID-19 Response Team
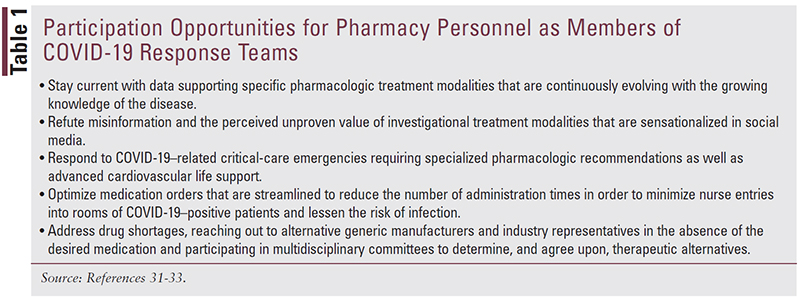
The training that pharmacists receive has uniquely positioned them to be members of the pandemic-response team, addressing drug shortages and refuting misinformation, among other tasks (TABLE 1). The additional, more obvious roles pharmacists have played, and continue to play, include swabbing, detection and surveillance, and oversight of appropriate storage of these new COVID-19 vaccinations. In terms of administration of vaccines, pharmacists must also offer education to optimize vaccine acceptance, as well as ensure that patients are appropriately screened for allergies and contraindications.34
Addressing Vaccine Hesitancy: Vulnerable Populations
Vaccine hesitancy is a factor among vulnerable populations in general, of whom those with SMI are a part. Since the pandemic disproportionately affects these populations and there is evidence that their mental health is affected by pandemic stress, it makes sense to emphasize addressing vaccine hesitancy as part of a strategy to control COVID-19 and improve community mental health.
One of the most significant roles the pharmacist can play at this time is to provide education to overcome vaccine hesitancy in the community as we strive to achieve herd immunity and a return to some degree of prepandemic normality. Vaccine hesitancy refers to refusal or delayed acceptance of vaccination despite the availability of vaccination services.35 Long before the COVID-19 vaccine was available, there was controversy about the need for vaccinations and the safety of immunizations and the preservatives contained within, particularly in children. Considered to be a complex controversy which is often vaccine-specific, researchers have reported that reluctance to become immunized can be influenced not only by lack of confidence but also by complacency and convenience.35
Healthcare experts and leaders within organizations such as the World Health Organization (WHO) have recognized, and have explored, context-specific causes of vaccine hesitancy and its impact in various settings. In collaboration with WHO, the Strategic Advisory Group of Experts (SAGE) on Immunization was established in 2012 to define the scope of hesitancy and to develop a plan to determine, define, and address the factors that influence behavioral decisions to reject or accept vaccination.36,37 It has been reported that using the term hesitancy could be negatively interpreted and that using alternative terminology such as vaccine confidence could foster a more positive approach, although the alternative term still covers concerns about vaccine safety, skepticism about those who make decisions about vaccine approvals, and compromised trust in those administering the vaccinations.36
Despite the excitement and anticipation of the eventual development of global herd immunity, surveys have indicated that many Americans are vaccine-hesitant, and according to John Whyte, MD, chief medical officer of the online health-information company WebMD, “While reports show increasing receptivity to getting a COVID vaccine, about one in five Americans still say they are not planning to get one, or would only if required,” he said, adding “the issue of vaccine hesitancy is also of particular concern in communities of color, which have been disproportionately impacted by the virus.”38
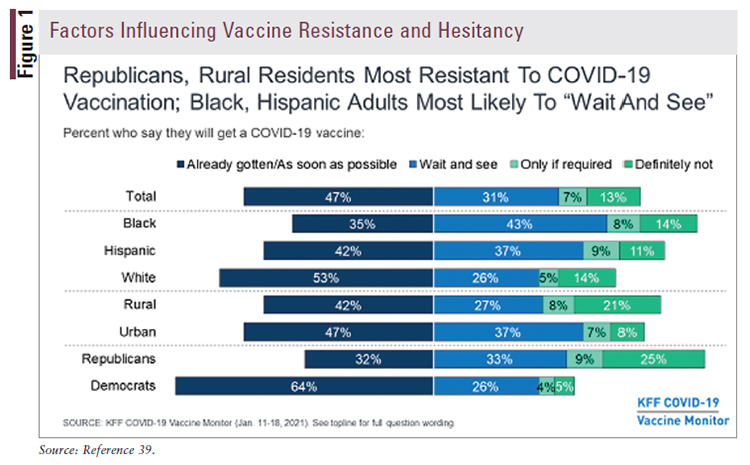
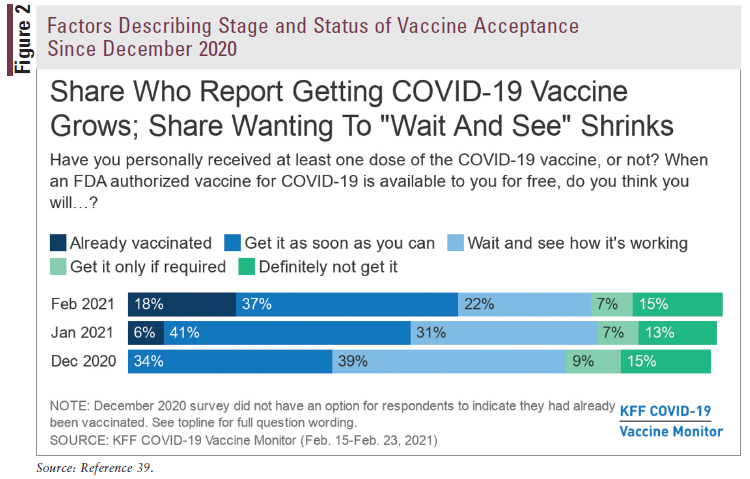
The highest rates of hesitancy are not just within communities of color. The Kaiser Family Foundation (KFF), a nonprofit health information and policy organization, reports that where an individual lives and their political persuasion, as well as ethnicity and cultural identity, also play a role in resistance or willingness to accept a vaccine, or waiting to see what happens next before considering accepting the vaccine (FIGURES 1 and 2).39
Jennings and colleagues explored vaccine hesitancy and reported that trust, belief in conspiracy theories, and spread of misinformation through social media were significant contributors to the phenomenon of declining a vaccine.40 The authors conducted a nationally representative survey of more than 1,400 adults that included five focus groups in December 2020 and reported that a key predictor of vaccine hesitancy was lack of trust. The distrust described included not only distrust in the vaccine itself but also distrust of the government agencies involved in the vaccine initiative.
The impact of social media was also notable, with researchers reporting that people who obtain information, especially misinformation, from relatively unregulated social media sources are particularly likely to be vaccine hesitant. The concept of accelerated vaccine development, concern about side effects and efficacy, and general conspiratorial beliefs all were also reported to increase the probability of “vaccine unwillingness.” It was conversely observed that trust in experts and health institutions decreases the vaccine hesitancy rate, so this is of key importance to pharmacists who are advocating for vaccination in the community.40
Racial and socioeconomic disadvantage has not only disproportionately influenced the impact of the morbidity and mortality of COVID-19 infection but has also negatively influenced the acceptance rates of black and Hispanic individuals for available vaccine.41 When compared with their white peers, these same groups reported a lower likelihood of having a close personal contact who has received the vaccine. Simply knowing someone who has been vaccinated for COVID-19 is associated with much higher vaccination rates with roughly half (52%) of those in the “vaccine as soon as possible,” group reporting that they know someone who has been vaccinated.41 This personal association is an important factor that should motivate pharmacists to share their personal immunization acceptance and also to encourage other vaccine recipients to share their vaccination acceptance and experience, even if they had mild symptoms from the injection.
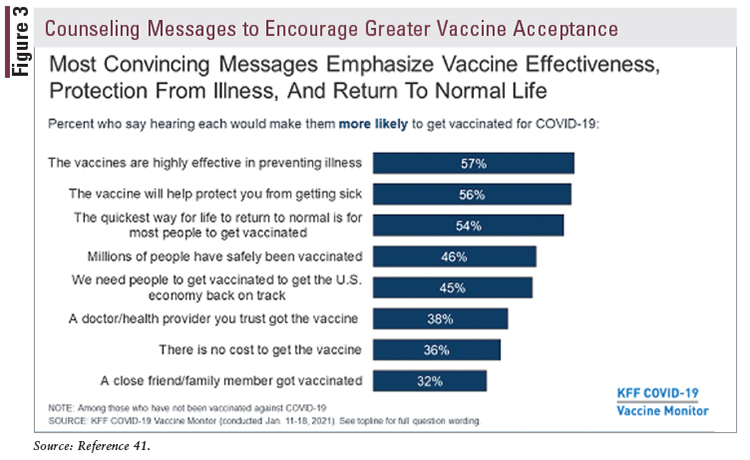
The KFF survey results demonstrate that enthusiasm and acceptance can be increased through messages that the public trusts and finds to be most convincing. Among these key messages are that the vaccine will prevent serious personal illness and will protect vulnerable contacts around them. The ability to see light at the end of the pandemic tunnel and return to a more normal life is another compelling motivational concept to promote greater energy in moving forward to achieving herd immunity (FIGURE 3).41
The KFF surveys also show that the vaccine-resistant express concerns about the safety of the new “fast-tracked” COVID-19 vaccine and of potential unknown side effects. Roughly half of the hesitant cite “lack of information” as their rationale, with higher shares of reluctance based on this gap in younger, black, and/or Hispanic adults (FIGURES 3and 4).41 And although it is generally accepted that the injection is associated with a degree of expected muscle soreness and mild flu-like symptoms, learning from someone in a trusted circle that they have experienced a serious allergic reaction, despite the rarity of the event, also further increases the reluctance for many people.41 Pharmacists can provide information regarding the rarity of serious adverse effects versus the more likely outcomes of morbidity and mortality caused by COVID-19, especially in people with chronic underlying conditions, including mental-health disorders, that compromise physical health and well-being. The KFF survey also supports previous findings that nurses, physicians, and other healthcare providers are considered the trusted source of information from whom they plan to seek opinion and healthcare consultation when deciding whether to be vaccinated. The pharmacist can play a significant role in educating the public in favor of vaccination; only about a quarter (26%) of patients have reported asking a healthcare professional about the vaccination to date.41
Addressing Vaccine Hesitancy: Ethical and Religious Reasons
Faith leaders have acknowledged the impressive success of vaccines despite the fact that all vaccines present health risks of one kind or another. These potential adverse outcomes have been just part of the debate and opposition to vaccination, which has been vigorous at times over the past century. As technology evolves, the origin and development of vaccines have become a more contentious debate, specifically the issue of what are referred to as “morally compromised cell lines.” The relevance of tissue origin is important for healthcare professionals to understand, regardless of their opinion about abortion, to offer a credible and empathetic consultation to patients who may be vaccine-resistant for this reason. As an effort to not diminish concerns about the sanctity of fetal lives lost, it is important to convey that it has been reported that those cell lines are maintained with the intent to sustain an indefinite life-span replicated in a laboratory that can be reproduced indefinitely. It has also been described that it is unlikely that any additional human cell lines will be produced or needed for vaccination development, which distinguishes it from fetal tissue transplantation that requires an additional supply of tissue, normally made available by further abortions.42
Two common human cell lines have provided cell cultures used in the production of vaccines. The WI-38 cell line and the other more commonly recognized line, MRC-5, were developed from tissue isolated after abortions performed in the 1960s. Fetal cells that have been multiplied into many new cells over the past 50-plus years have resulted in the establishment of fetal-cell lines.
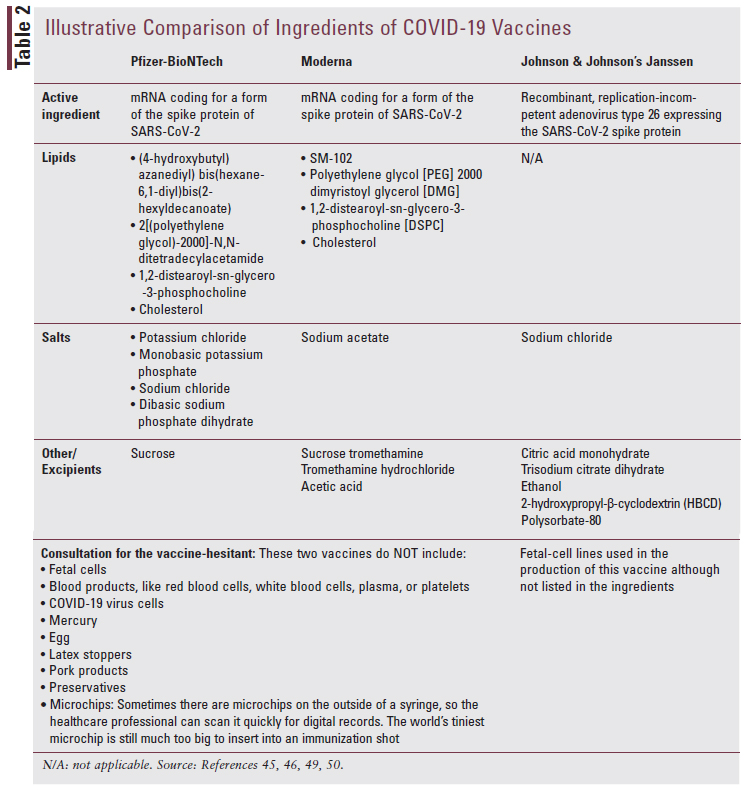
Current fetal-cell lines are reported to be thousands of generations removed from the original fetal tissue and may be used for any stage of vaccine development, confirmation to ensure the vaccine works, and production—the actual manufacturing of the final product.43 More recently, with the development of the COVID-19 vaccine, the Human Embryonic Kidney (HEK) 293 emerged as the preferred fetal-cell line for this vaccine.44 All HEK 293 cells are reported to be distant descendants, remote and indirectly connected to tissue derived from an elective abortion in the 1970s that took place in the Netherlands. The COVID-19 vaccine being developed by Oxford University and the pharmaceutical company AstraZeneca is commonly referred to as the “Oxford vaccine.” In media press releases, researchers involved in the discovery of the Oxford vaccine described these cell lines as laboratorycultivated “descendants” of the cells originally obtained.44 Manufacturers for both the Pfizer and Moderna vaccines used HEK 293 fetal-cell lines only for the confirmation phase to ensure the vaccines functioned properly and effectively, but they did not use them during the development or production phases, and therefore, they are not included in the final vaccine formulation.45,46 The Oxford vaccine used HEK 293 cells to grow the vaccine and published specific details on manufacturing, with assurance that the vaccine itself would contain neither fetal cells nor fetal DNA.47 Johnson & Johnson used a different cell line called PER.C6, also derived from fetal cells, in production and confirmation phases to test its vaccine’s effectiveness against COVID-19 (TABLE 2).45,46,48-50
It is necessary to professionally validate, however, that some vaccines, such as Varivax and Zostavax (although no longer the preferred shingles vaccine), for example, do contain residual components of MRC-5 cells including DNA and protein, which are considered excipients and not active ingredients contributing to the effectiveness of the vaccine.49
Common Religious and Ethical Vaccine Concerns
The Vatican’s Catholic Pontifical Academy for Life reaffirmed in 2017 what they originally decided in 2005, that in the absence of alternatives, Catholics could, in good conscience, receive vaccines made using historical human fetal-cell lines.51,52 The beliefs and practices of various religious groups can seemingly be in conflict with some additional components of vaccines beyond that of the fetal-cell lines. Some vaccines contain components with porcine (pork) origins, and religions that oppose the use of pork products may also have objections to vaccination based on this ingredient. A 1995 decision rendered and published by the Islamic Organization for Medical Sciences states, “The gelatin formed as a result of the transformation of the bones, skin and tendons of a judicially impure animal is pure, and it is judicially permissible to eat it.”53
For those of Jewish faith, drugs of porcine origin are derived from the pancreas which, as extracted, is not edible in the food sense, and for excipients (nonactive ingredients in vaccines) such as gelatin, if no alternative is available, consumption of gelatin is permitted because it is being consumed in a nonedible form.51 The acceptability of these dietary components when eaten under these conditions extrapolates permission to allow parenterally administered medications containing the same essential components.
The COVID-19 vaccine developed by Pfizer does not contain any components of animal origin and has been declared halal based on the information available.54,55 Halal is an Arabic word that means “lawful or allowed,” which is the opposite of haram, which means “unlawful or not allowed” in the Islamic religion.56 Even though cholesterol is listed in the ingredients, all lipid excipients used in COVID-19 mRNA vaccine BNT162b2 are either from plant-derived sources or are synthetic. The vaccine contains no animal components.54
It is important to remember that religious and ethical refusal is a very sensitive and important topic within faith communities. The pharmacist, in collaboration with the rest of the healthcare team, should encourage each patient to ask questions to feel reassured that they are making a decision that is based on not only their health, or the health of their family, but also the health of society. It may be necessary for additional referrals to discuss ethical and religious concerns with faith leaders and also to provide the evidence-based factual information that is available to address these religious concerns, such as that provided by the Immunization Action Coalition.42 Vaccine recipients or candidates considering vaccination should feel like they are making a fully informed decision, which may require not only discussing the risks and benefits of the COVID-19 vaccines with their doctor but also potentially a personal conversation with a faith leader about ethical, moral, and religious concerns they may have.
Conclusion
The stress of the COVID-19 pandemic has affected everyone in the community; however, the negative impact has been more significant for patients challenged with health disparities and pre-existing vulnerabilities such as mental-health issues. Pharmacists are key members of the healthcare team that will collaboratively lead communities out of the pandemic by educating where there are knowledge gaps and uncertainties, including vaccine hesitancy, which can impede our goal of achieving population immunity and a postpandemic future.
REFERENCES
1. Ptacek R, Ptackova H, Martin A, Stefano GB. Psychiatric manifestations of COVID-19 and their social significance. Med Sci Monit. 2020;26:e930340.
2. Gandhi RT, Lynch JB, del Rio C. Mild or moderate Covid-19. N Engl J Med. 2020;383(18):1757-1766.
3. Lavezzo E, Franchin E, Ciavarella C, et al. Suppression of a SARSCoV-2 outbreak in the Italian municipality of Vo’. Nature. 2020;584(7821):425-429.
4. Berlin DA, Gulick RM, Martinez FJ. Severe Covid-19. N Engl J Med. 2020;383(25):2451-2460.
5. Wiersinga WJ, Rhodes A, Cheng AC, et al. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324(8):782-793.
6. Whittaker A, Anson M, Harky A. Neurological manifestations of COVID-19: a systematic review and current update. Acta Neurol Scand. 2020;142(1):14-22.
7. Correa-Palacio AF, Hernandez-Huerta D, Gómez-Arnau J, et al. Affective psychosis after COVID-19 infection in a previously healthy patient: a case report. Psychiatry Res. 2020;290:113115.
8. Chandra PS, Shiva L, Nagendrappa S, et al. COVID 19 related psychosis as an interface of fears, socio-cultural issues and vulnerability: case report of two women from India. Psychiatry Res. 2020;290:113136.
9. Mawhinney JA, Wilcock C, Haboubi H, Roshanzamir S. Neurotropism of SARS-CoV-2: COVID-19 presenting with an acute manic episode. BMJ Case Rep. 2020;13(6):e236123.
10. Epstein D, Andrawis W, Lipsky AM, et al. Anxiety and suicidality in a hospitalized patient with COVID-19 infection. Eur J Case Rep Intern Med. 2020;7(5):001651.
11. Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):e21.
12. Centers for Medicare & Medicaid Services. Fact sheet: service use among Medicaid & CHIP beneficiaries age 18 and under during COVID-19. www.cms.gov/newsroom/fact-sheets/fact-sheet-service-use-amongmedicaid-chip-beneficiaries-age-18-and-under-during-covid-19. Accessed February 24, 2020.
13. Leeb RT, Bitsko RH, Radhakrishnan L, et al. Mental health–related emergency department visits among children aged <18 years during the COVID-19 pandemic—–United States, January 1–October 17, 2020. www.cdc.gov/mmwr/volumes/69/wr/mm6945a3.htm. Accessed February 24, 2021.
14. Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130140.
15. Kim SW, Su KP. Using psychoneuroimmunity against COVID-19. Brain Behav Immun. 2020;87:4-5.
16. Szczesniak D, Gladka A, Misiak B, et al. The SARS-CoV-2 and mental health: from biological mechanisms to social consequences. Prog Neuropsychopharmacol Biol Psychiatry. 2021;104:110046.
17. Wand APF, Zhong BL, Chiu HFK, et al. COVID-19: the implications for suicide in older adults. Int Psychogeriatr. 2020;32(10):1225-1230.
18. CDC. Coping with stress. www.cdc.gov/coronavirus/2019-ncov/ daily-life-coping/managing-stress-anxiety.html. Accessed February 18, 2021.
19. CDC. Healthcare personnel and first responders: how to cope with stress and build resilience during the COVID-19 pandemic. www.cdc. gov/coronavirus/2019-ncov/hcp/mental-health-healthcare.html. Accessed February 24, 2021.
20. Panchal N, Kamal R, Cox C, Garfield R. The implications of COVID19 for mental health and substance use. Kaiser Family Foundation. February 10, 2021. www.kff.org/coronavirus-covid-19/issue-brief/theimplications-of-covid-19-for-mental-health-and-substance-use. Accessed April 18, 2021.
21. Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;113(10):707-712.
22. Nemani K, Li C, Olfson M, et al. Association of psychiatric disorders with mortality among patients with COVID-19. JAMA Psychiatry. 2021;78(4):380-386.
23. CDC. COVID-19 racial and ethnic health disparities. www.cdc.gov/ coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/ index.html. Accessed February 18, 2021.
24. Clausen W, Watanabe-Galloway S, Baerentzen MB, Britigan DH. Health literacy among people with serious mental illness. Community Ment Health J. 2016;52(4):399-405.
25. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. National action plan to improve health literacy. https://health.gov/sites/default/files/2019-09/Health_Literacy_ Action_Plan.pdf. Accessed April 18, 2021.
26. Schoeyen HK, Birkenaes AB, Vaaler AE, et al. Bipolar disorder patients have similar levels of education but lower socio-economic status than the general population. J Affect Disord. 2011;129(1-3):68-74.
27. Krishan S, von Esenwein SA, Druss BG. The health literacy of adults with severe mental illness. Psychiatr Serv. 2012;63(4):397.
28. American Diabetes Association. New data highlights severe health and economic impact of pandemic on millions living with diabetes. July 29, 2020. www.diabetes.org/newsroom/press-releases/2020/new-datahighlights-severe-health-and-economic-impact-of-pandemic-on-millionsliving-with-diabetes. Accessed February 24, 2021.
29. Hill-Briggs F, Adler NE, Berkowitz SA, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care. 2020;44(1):258279.
30. Penninx BWJH, Lange SMM. Metabolic syndrome in psychiatric patients: overview, mechanisms, and implications. Dialogues Clin Neuroscience. 2018;20(1):63.
31. Li M, Razaki H, Mui V, et al. The pivotal role of pharmacists during the 2019 coronavirus pandemic. J Am Pharm Assoc. 2020;60(6):e73-e75.
32. Wilner T, Holton A. Breast cancer prevention and treatment: misinformation on Pinterest, 2018. Am J Public Health. 2020;110(S3):S300-S304.
33. Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and hospital mortality rates. Pharmacotherapy. 2007;27(4):481-493.
34. Murphy KR, Patel NC, Ein D, et al. Insights from American College of Allergy, Asthma, and Immunology COVID-19 Vaccine Task Force: allergic reactions to mRNA SARS-CoV-2 vaccines. Ann Allergy Asthma Immunol. 2021;126(4):319-320.
35. MacDonald NE, SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):41614164.
36. World Health Organization. Immunization, vaccines and biologicals: policy recommendations. www.who.int/immunization/policy/en/. Accessed February 24, 2021.
37. World Health Organization. Immunization, vaccines and biologicals: SAGE working group dealing with vaccine hesitancy (March 2012 to November 2014). www.who.int/immunization/sage/sage_wg_vaccine_ hesitancy_apr12/en/. Accessed February 25, 2021.
38. New COVID-19 vaccine misinformation center launches. U.S. Pharmacist. February 10, 2021. www.uspharmacist.com/article/newcovid19-vaccine-misinformation-center-launches. Accessed February 26, 2021.
39. Kaiser Family Foundation. Vaccine monitor: nearly half of the public wants to get a COVID-19 vaccine as soon as they can or has already been vaccinated, up across racial and ethnic groups since December. January 27, 2021. www.kff.org/coronavirus-covid-19/press-release/ vaccine-monitor-nearly-half-of-the-public-wants-to-get-covid-19-vaccineas-soon-as-they-can-or-has-already-been-vaccinated-up-across-racial-andethnic-groups-since-december/. Accessed February 25, 2021.
40. Jennings W, Stoker G, Willis H, et al. Lack of trust and social media echo chambers predict COVID-19 vaccine hesitancy. medRxiv. January 27, 2021. www.medrxiv.org/content/10.1101/2021.01.26.21250246v1. Accessed April 19, 2021.
41. Hamel L, Kirzinger A, Lopes L, et al. KFF COVID-19 Vaccine Monitor: January 2021: vaccine hesitancy. www.kff.org/report-section/ kff-covid-19-vaccine-monitor-january-2021-vaccine-hesitancy. Accessed February 26, 2021.
42. Immunization Action Coalition. Religious concerns: talking about vaccines: religious concerns. www.immunize.org/talking-about-vaccines/ religious-concerns.asp. Accessed February 27, 2021.
43. Lawler J. You asked, we answered: do the COVID-19 vaccines contain aborted fetal cells? www.nebraskamed.com/COVID/you-asked-weanswered-do-the-covid-19-vaccines-contain-aborted-fetal-cells. Accessed February 27, 2021.
44. Australian Associated Press. Are ‘aborted babies’ being used for a COVID-19 vaccine? October 22, 2020. www.aap.com.au/are-abortedbabies-being-used-for-a-covid-19-vaccine. Accessed February 27, 2021.
45. FDA. Fact sheet for healthcare providers administering vaccine (vaccination providers): emergency use authorization (EUA) of the PfizerBioNTech COVID-19 vaccine to prevent coronavirus disease 2019 (COVID-19). www.fda.gov/media/144413/download. Accessed April 18, 2021.
46. FDA. Fact sheet for healthcare providers administering vaccine (vaccination providers): emergency use authorization (EUA) of the Moderna COVID-19 vaccine to prevent coronavirus disease 2019 (COVID-19). www.fda.gov/media/144637/download. Accessed April 18, 2021.
47. Wu S, Zhong G, Zhang J, et al. A single dose of an adenovirusvectored vaccine provides protection against SARS-CoV-2 challenge. Nat Commun. 2020;11(1):4081.
48. Janssen. Our innovative vaccine technology platforms–ADVAC® and PER.C6®. www.janssen.com/emea/emea/janssen-vaccine-technologies. Accessed April 7, 2021.
49. CDC. Vaccine excipient summary: excipients included in U.S. vaccines, by vaccine. www.cdc.gov/vaccines/pubs/pinkbook/downloads/appendices/b/ excipient-table-2.pdf. Accessed February 27, 2021.
50. FDA. Fact sheet for recipients and caregivers: emergency use authorization (EUA) of the Janssen COVID-19 vaccine to prevent coronavirus disease 2019 (COVID-19) in individuals 18 years of age and older. https://www. fda.gov/media/146305/download. Accessed April 7, 2021.
51. Institute for Vaccine Safety. Religion and vaccines. www.vaccinesafety. edu/Religion.htm. Accessed February 27, 2021.
52. Pontifical Academy for Life. Moral reflections on vaccines prepared from cells derived from aborted human fetuses. Natl Cathol Bioeth Q. 2006;6(3):541-537.
53. Immunize.org. Judicially prohibited and impure substances in foodstuff and drugs [Islam]. www.immunize.org/talking-about-vaccines/porcine. pdf. Accessed February 27, 2021.
54. Medicines and Healthcare Regulatory Agency [UK]. Regulatory approval of Pfizer/BioNTech vaccine for COVID-19. https://www.gov. uk/government/publications/regulatory-approval-of-pfizer-biontech-vaccinefor-covid-19. Accessed February 27, 2021.
55. Mahmood B. Fact check: is Pfizer COVID-19 vaccine not halal, as viral video claims? December 18, 2020. https://www.newsweek.com/ fact-check-pfizer-covid-19-vaccine-halal-1555998. Accessed February 27, 2021.
56. American Halal Foundation. What is halal food? https://halalfoundation. org/what-is-halal-food/. Accessed February 27, 2021.