Population Health and Social Determinants of Health in Diabetes Management
RELEASE DATE
November 1, 2020
EXPIRATION DATE
November 30, 2022
FACULTY
Donna M. Lisi, PharmD, BCPS, BCACP, BCGP, BCPP
Clinical Pharmacist, Long Term/Post-Acute Care
Hackensack Meridian Health
Eatontown, New Jersey
FACULTY DISCLOSURE STATEMENTS
Dr. Lisi has no actual or potential conflicts of interest in relation to this activity.
Postgraduate Healthcare Education, LLC does not view the existence of relationships as an implication of bias or that the value of the material is decreased. The content of the activity was planned to be balanced, objective, and scientifically rigorous. Occasionally, authors may express opinions that represent their own viewpoint. Conclusions drawn by participants should be derived from objective analysis of scientific data.
ACCREDITATION STATEMENT
 Pharmacy
Pharmacy
Postgraduate Healthcare Education, LLC is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education.
UAN: 0430-0000-20-130-H01-P
Credits: 2.0 hours (0.20 ceu)
Type of Activity: Knowledge
TARGET AUDIENCE
This accredited activity is targeted to pharmacists. Estimated time to complete this activity is 120 minutes.
Exam processing and other inquiries to:
CE Customer Service: (800) 825-4696 or cecustomerservice@powerpak.com
DISCLAIMER:
Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patients’ conditions and possible contraindications or dangers in use, review of any applicable manufacturer’s product information, and comparison with recommendations of other authorities.
GOAL
To educate the pharmacist about the principles of population-health–based social determinants of health and their application in the management of the patient with diabetes.
OBJECTIVES
After completing this activity, the participant should be able to:
- Describe what is meant by population health.
- List the Healthy People 2030 objectives and goals for the management of diabetes.
- Describe the six social determinants of health
and how they pertain to the management of
patients with diabetes. - Identify opportunities for the pharmacist to address social determinants of health to optimize the care of patients with diabetes.
ABSTRACT: Diabetes is a major source of morbidity and mortality in the United States and the seventh most common cause of death. The number of persons with diabetes is projected to markedly increase in the coming years. Even among those who are diagnosed, glycemic control is often inadequate. Pharmacists can individualize care and address the diabetes-management issues that are most important to patients’ physical and mental well being by adopting a population-health–based approach focusing on social determinants of health such as economic stability, neighborhood/physical environment, education, food, community/social context, and local healthcare systems.
According to the CDC, population health is an interdisciplinary, customizable approach that “brings significant health concerns into focus and addresses ways that resources can be allotted to overcome the problems that drive poor health conditions in the population.”1 It is based on the principles of social determinants of health (SDH), which are conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.2
On August 18, 2020, the U.S. Department of Health and Human Services released Healthy People 2030 (HP 2030), a set of science-based, 10-year national objectives for improving health and wellbeing in the United States.3 The HP 2030 diabetes management goal is to reduce disease burden and improve the quality of life for all persons who have, or are at risk for, diabetes.4 The HP 2030 objectives for diabetes, baseline statistics, and target goals are found in TABLE 1.
In addition, there are two developmental diabetes objectives. Developmental objectives represent high priority issues that do not have reliable baseline data or evidence-based interventions available.4 The goals of these developmental objectives are to reduce the rate of all-cause mortality and the rate of cardiovascular-disease deaths among persons with diabetes. Two other objectives that are being tracked for informational purposes only include reducing the rate of lower-extremity amputations in persons with diagnosed diabetes and monitoring the proportion of the diabetic population with a glycosylated hemoglobin A1C (HbA1C) value less than 7%.4 These HP 2030 diabetes goals and objectives offer yet another opportunity for pharmacists to play a vital role in the management of patients with diabetes.
PATIENT-CENTERED DIABETES MANAGEMENT IN THE SOCIAL CONTEXT
The 2020 National Diabetes Statistics Report has indicated that 34.2 million people, or 10.5% of the U.S. population, have diabetes.5 This number is expected to increase to 39.7 million or 13.9% in 2030, and up to 60.6 million or 17.9% of the population by 2060.6 It is currently the seventh leading cause of death in the U.S.7 Even when patients are diagnosed, their disease may not be adequately controlled—18% of adults have an HbA1C greater than 9%.8 Increases in percent prevalence will continue in all patient populations, but especially among those aged 65 years or older and people of color, with black women, followed by black men, having the highest rates of diabetes.6
Another study found that childhood environment, education, socioeconomic status, gender, and the culture of public health were SDH that contributed to poorer health outcomes in patients with type 1 diabetes who progressed to end-stage renal disease. Participants in this study expressed the concern that healthcare providers focused only on the management of diabetes without considering the myriad of daily challenges that they faced living with a chronic illness. It is important to recognize that individual health behaviors can be positively or negatively affected by societal structures and forces, which are embodied in SDH.9 A systematic review found that SDH not only affect glycemic control in type 2 diabetes but also impact low-density lipoproteins and blood pressure control, which ultimately affect the progression of diabetes.10
These statistics point to an increase in burden both from a humanistic and a societal perspective. Applying population health principles—in particular, assigning actionable interventions to the SDH that can be directly impacted by pharmacists—may play a role in reducing this burden. Since the early days of the Ashville Project and its role in the National Diabetes Prevention Program, pharmacists have demonstrated that they can positively impact the health of persons with diabetes while containing costs.11,12 However, health inequities within diabetes management are well documented, pointing to the need for a more systematic approach to address these disparities.
The 2020 American Diabetes Association (ADA) Standards of Care recognize the association between social and environmental factors and the prevention and treatment of diabetes and call for tailoring diabetes management within the social context.13 The Consensus Report of the ADA, the Association of Diabetes Care and Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of Physician Assistants, the American Association of Nurse Practitioners, and the American Pharmacists Association on diabetes self-management education and support in adults with type 2 diabetes advocates for identifying SDH such as food access, financial means, health literacy and numeracy, social support systems, and health beliefs and attitudes in managing patients with diabetes.14 In recognition of the importance of SDH, there has been a call for all diabetes clinical-practice guidelines to include recommendations to evaluate SDH in order to provide patient-centered care.15 As has been eloquently stated, “While professionals are experts about diseases and the recommended course of action, patients are experts about their own lives.”16 Both professional and personal insights have to be married in order to meet the needs of patients with diabetes.
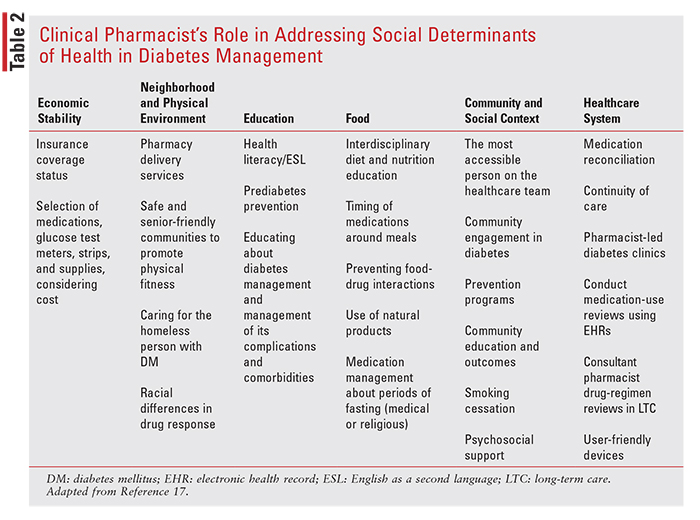
A schema has been proposed to assist the clinical pharmacist in systematically addressing SDH in order to enhance the delivery of patient care (TABLE 2). This schema serves as an example of some of the interventions that pharmacists can be involved in when caring for their patients with diabetes. Phar macists can optimize diabetes medication regimens by individualizing drug therapy based on SDH needs. Among the SDH addressed are 1) economic stability; 2) neighborhood and physical environment; 3) education; 4) food; 5) community and social context; and 6) healthcare system.17
SOCIAL DETERMINANTS OF HEALTH AND DIABETES
Economic Stability
A recent study conducted in an urban diabetes center found that one in four patients reported cost-related insulin underuse, which was associated with poor glycemic control. Furthermore, about two-thirds could not afford diabetes supplies. In over one-third of cases, healthcare providers were not aware of their patients’ reason for nonadherence.18 Partly driving this cost issue has been the rapid rise in the price of U500 insulin, a concentrated form of insulin which is being more widely used in patients in whom it is difficult to achieve glycemic control, such as overweight or obese patients.19 To address this issue, in 2018 the ADA commissioned a study to examine the affordability of insulin. The study found that patients frequently had to choose between buying medications or food or keeping doctor’s appointments and paying for housing costs.20
Poor socioeconomic status often leads to low self-esteem, stress, and feelings of powerlessness, which can impact a patient’s engagement in diabetes self-management.9,21 Lower socioeconomic status has an inverse relationship with mortality and diabetes complications.21 A longitudinal study of older adults with diabetes found that economic instability and diffi culty paying bills were an even greater risk factor for poor glycemic control than were psychosocial or neighborhood factors.22
The COVID-19 pandemic is having a major negative financial impact on patients with diabetes. According to an online survey of 5,000 patients with diabetes that was conducted in June 2020, 18% were unemployed (vs. 12% of nondiabetics), and one in four patients used their savings, took out a loan, or used their stimulus money to pay for their insulin—or they simply rationed their dose of insulin. Those who were low-income were particularly hard hit, with about 50% losing some or all of their income. This also occurred in up to 70% of self-employed patients with diabetes. This is significant given that the loss of employment is often accompanied by discontinuation of medical and prescription coverage. This economic instability is adding to the stress of the pandemic and has contributed to food insecurity and depression. Couple this with the inability to exercise and the increased risk of having a severe outcome if infected with COVID-19 and it becomes clear that the burden of this pandemic is disproportionately impacting those with diabetes.23
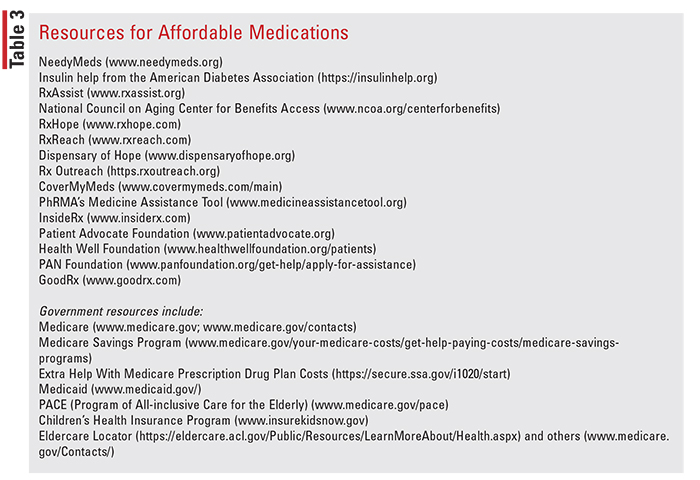
Pharmacists can play a major role in assisting patients in identifying affordable sources of medication. Numerous resources are available to help expand access to care (TABLE 3).
Neighborhood and Physical Environment
One novel approach to assessing a community’s degree of social vulnerability to diabetes involves applying a population-based approach. 24 Social vulnerability refers to “the resilience of communities when confronted by external stresses on human health, stresses such as natural or human-caused disasters, or disease outbreaks.”25 Using multivariate profiles, which were based on 35 socioeconomic indicators associated with adult residents with type 2 diabetes in a given community, the vulnerability of the community to being on “the path to diabetes” was assessed. This approach can be used to target community-based prevention measures in neighborhoods with high concentrations of residents manifesting the composite vulnerability profile.24 Supermarket density based on zip code, another epidemiological factor, has been found to inversely correlate with diabetes risk.26
Neighborhood and physical environment can impact diabetes self-care and access to medications. One study of African Americans with diabetes found that poor glycemic and hypertension control were correlated with living in a highly segregated neighborhood, but this effect was mitigated in a more walkable neighborhood.27 Distance to a pharmacy, walkability, recreational facilities, neighborhood aesthetics, and the safety of a neighborhood can play a role in adherence.28 Fortunately, pharmacy chains and many local independent pharmacies offer delivery service. GetMyRx (www.getmyrx.com), a free service, partners with independent pharmacies to increase access to care.
Another tool is the use of telehealth and telepharmacy.13 Telepharmacy initiatives as simple as using a personalized, secure online portal that is part of the electronic health record or as complex as a telephonic diabetes management program have been associated with improved glycemic control.29,30
Age-friendly environments, which is a concept promoted as part of an international effort by the World Health Organization to help cities prepare for aging populations and trends in urbanization, has focused on issues such as housing, caregiving, community engagement, volunteering, social inclusion, and combating isolation among older adults, services that are needed now more than ever in the COVID-19 era. The American Association of Retired Persons (AARP) has developed a network of age-friendly states and communities to help older adults age in place.31 Pharmacists can support such efforts at the local and county level by working with councils on aging and local AARP chapters.
Another factor that can affect the management of diabetes is homelessness. The ADA estimates that the prevalence of diabetes in the homeless population is about 8%.13 Homeless patients face many challenges including food insecurity, lack of insurance, inability to safely store their diabetes medications and supplies, and lack of proper storage temperatures. Additionally, many homeless patients suffer from mental health issues.13 Programs such as Dispensary of Hope provide free medications to patients who cannot afford them. Approximately 19% of veterans are homeless; veteran centers may assist in securing diabetes medications and supplies.32 Pharmacists can provide services at local free clinics.33 Recommendations are available to assist clinicians in providing care to people who are homeless and have diabetes.34
Another factor that is often tied to neighborhoods is race. Racial inequities have been found in both health and housing. Living in a poor neighborhood increases the odds of having diabetes for blacks as well as whites.35,36 Pharmacists can screen patients who are of lower socioeconomic means for potential barriers to care.
Tied to race is the issue of pharmacogenomics. While personalized medicine is still in an early stage with regard to the management of diabetes, differences have been observed in response to metformin and, to a lesser extent, with sulfonylureas, thiazolidinediones, and dipeptidyl peptidase-4 (DPP-4) inhibitors.37 Pharmacogenomic studies involving antidiabetic agents are fraught with methodological flaws including observational design, small sample sizes, and small effect sizes.
The most studied form of diabetes with respect to pharmacogenomics is maturity-onset diabetes of the young (MODY), which typically begins before age 25 years and only accounts for about 3% of diabetes cases. MODY is most commonly associated with a mutation in the gene HFNF1A (hepatocyte nuclear factor-1 alpha), which makes these patients extremely responsive to low doses of sulfonylureas, the drugs of choice to treat this condition.37
Overall, metformin is the most pharmacogenomically studied hypoglycemic agent. In patients receiving metformin, a decrease of 0.5% in HbA1C is seen in patients with reduced solute carrier 2 member 2/ glucose transporter 2 (SLC2A2/GLUT2) transporter function. Reductions in organic cation transporter 1 (OCT1) transporter, plasma membrane monoamine transporter (PMAT) expression, and serotonin transporter (SERT) genotype are associated with an increase in adverse gastrointestinal effects.37 Racial differences have been seen in response to metformin, with African Americans having an average reduction in HbA1C of 0.9% compared with 0.42% in European Americans.38 Sulfonylureas are affected by genetic polymorphism of CYP2C9. There is a 3.44 times greater response to sulfonylureas in patients with CYP2C9*2 and CYP2C9*3 alleles, as this is associated with reduced clearance of the oral hypoglycemics. Therapeutic response to rosiglitazone (i.e., decrease in HbA1C) and adverse effects are influenced by CYP2C9 and solute carrier organic anion transporter family member 1B1 (SLCO1B1) activity. Little is known about the pharmacogenomics of DPP-4 inhibitors, but there appears to be a 0.5% reduction in HbA1C due to variations in chymotrypsinogen B1/2 (CTEB1/2).37 Recently, polymorphisms involving glucagon-like peptide-1 receptor agonists (GLP1 RA) have been reported.39
Education
There appears to be a direct correlation between education and genetic risk scores for developing diabetes, with increased schooling being associated with lower HbA1C levels, especially prior to the initiation of medication. A lower educational level may correlate with poorer socioeconomic status and living in neighborhoods with less access to healthy food choices.40
Adequate health literacy is necessary for patients to engage in diabetes self-management.41 Poor health literacy has been associated with worse glycemic control, higher rates of retinopathy, reduced healthcare access, and inadequate diabetes self-management.42,43 A small study conducted among African American women in Arizona confirmed that health literacy as well as education and economic factors directly influenced diabetes self-management.44 There is an improvement in glycemic control when health literacy is addressed.43
A major role of the pharmacist is education. Pharmacists have been actively involved in the National Diabetes Prevention Program.12 Educational programs promoting self-management for patients with low health-literacy skills can reduce disparities in diabetes outcomes and improve glycemic control.45,46 In addition to educating patients about their diabetes medications, pharmacists serve as patient advocates by promoting age and disease-appropriate immunizations.47 Patient education should also focus on smoking cessation (if applicable), weight reduction, increasing physical activity, the importance of monitoring HbA1C and blood glucose levels, and promoting adherence to antihypertensive and antilipidemic regimens. Pharmacists can avail themselves of health-literacy training programs through the CDC and familiarize themselves with simple screening tools that can identify limited health literacy.48,49
Pharmacists should also be cognizant of language barriers that may lead to ineffective communication with their patients.13 HealthReach is an open-access database created through a national collaborative partnership with the National Institutes of Health and hospitals, clinics, community health centers, voluntary organizations, government agencies, academic institutions, and national nongovernmental organizations that provides free, multicultural health information and patient-education materials for patients with limited English proficiency.50 Another resource, the National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care (National CLAS Standards) provides strategies to reduce language barriers, develop cultural competency, and address deficiencies in health literacy to improve patient care for non–English-speaking patients.51
Food
There are multiple areas of diabetes management that involve food, and the pharmacist can play an active role in both education and counseling. Food insecurity, which refers to “the unreliable availability of nutritious foods and the inability to consistently obtain food without resorting to socially unacceptable practices” occurs in up to 20% of those with diabetes.13 Pharmacists should discretely broach the subject and offer to refer the patient to local social services including governmental programs and local food banks should this be a concern. Food is increasingly being viewed as medicine in the management of chronic illnesses. Pharmacists can encourage healthy eating habits and reinforce nutritional guidelines for diabetes management.52 Meal-planning resources such as Counting Carbs or the Plate Method are readily available.53
Another area impacted by food is the timing of medication administration. Sulfonylureas should be given before meals. Acarbose is administered with the first bite of food. Metformin should be administered with meals to reduce gastrointestinal intolerance, and the meglitinides should be taken before meals.54 For insulins other than basal insulin, patients should be aware of how meals can impact their glycemic control and episodes of hypoglycemia.55
Pharmacists can be involved in counseling patients on medication administration and on how to take care of themselves if they become sick.56 With cultural sensitivity in mind, pharmacists can also guide patients on medication regulation during religious holidays that involve fasting.57
As part of a team effort, pharmacists can work with dieticians to educate patients about food-drug interactions such as the administration of rapaglinide with grapefruit juice or sulfonylureas with alcohol.
Patients on long-term metformin therapy should be screened for vitamin B12 deficiency.54
Patients with diabetes are 1.6 times more likely to use alternative medicines than are patients without diabetes. These are often in the form of dietary supplements, which have the potential to interact with other medications. Chromium can interfere with levothyroxine, and zinc interacts with fluoroquinolones.58
Community and Social Context
Addressing mental health issues is important in diabetes care. There appears to be a direct relationship between psychosocial SDH (such as psychological distress, social support, and self-efficacy) and glycemic control and diabetes self-care. However, the psychosocial effects appear to be independent of self-care, indicating that multicomponent interventions that address both psychosocial interventions and self-care training may be needed.59,60
As our nation reckons with issues of systemic racism, the impact of racial/ethnic differences in diabetes clinical outcomes and the role that SDH play in affecting these outcomes needs to be more clearly defined. Although data are limited, minority youth with diabetes may be most particularly affected by healthcare disparities, as they often face issues involving low family income and family burden that can adversely affect their quality of life.61 Perceived discrimination impacts quality of life and self-care.28 Pharmacists should be culturally sensitive to the needs of their patients.
One in four patients with diabetes suffers from depression, and up to 45% of patients experience distress related to their illness.62 This distress can be further exacerbated since patients with diabetes are more likely to experience severe disease secondary to COVID-19. Furthermore, there is a bidirectional interaction between COVID-19 and diabetes, manifesting as both an increased risk of severe infection and new-onset diabetes accompanied by severe metabolic complications, including diabetic ketoacidosis.63 Even before the COVID-19 pandemic, half of patients with diabetes perceived that they were under financial stress and about 20% reported financial insecurity affecting both healthcare access and food insecurity, resulting in cost-related nonadherence.64
Pharmacists can play an active role in assisting with the recommendation of insulin doses, which are often very high in the presence of ketoacidosis. In addition, because pharmacists are the most accessible members of the healthcare team, they are in a position to screen and refer patients who are in need of psychosocial support, especially during this pandemic.65,66 Also, assisting patients with their medication-related financial needs by suggesting the use of lower-cost drugs such as metformin can reduce stress and address cost barriers while maintaining a therapeutic regimen. Purchasing prescriptions from overseas, which is often done in an attempt to save money, has not been shown to alleviate cost-related nonadherence.64
For those patients with diabetes who are on psychotropics, especially antipsychotics, monitoring for weight gain, lipid abnormalities, and increased hyperglycemia is essential, because these can lead to nonadherence and adverse cardiovascular outcomes.67-69 Pharmacists can make recommendations for diabetes and psychiatric pharmacologic and nonpharmacologic interventions based on individualized patient-care needs.
Healthcare System
The healthcare system offers a myriad of opportunities for pharmacists to address SDH among their patients with diabetes.
A recent study found that most factors that influence glycemic control such as insulin use, smoking status, self-efficacy, and medication adherence are mutable and amenable to interventions by the healthcare system. It called for the implementation of pharmacist-based interventions where pharmacists partner with patients to develop treatment plans or collaborate with physicians as part of team-based care.70
One of the most important means of pharmacist involvement is through medication reconciliation during transitions of care (TOC), which improves both patient safety and quality of care.71 Pharmacists can help the team navigate TOC and avoid miscommunication, assist with patient education, and help prevent accountability breakdowns, which have been identified by the Joint Commission as causes of ineffective TOC.72 Pharmacists can also assess patients’ ability to afford their medications at this time.
In primary care, pharmacist-led diabetes clinics point to the value of the clinical pharmacist in leading or managing diabetes teams, services, or clinics and show that pharmacist involvement in the management of diabetes improves patient care.73-77
In the hospital setting, pharmacists can conduct drug reviews or audits using the electronic health record to examine not only prescribing patterns for appropriateness of antidiabetic medications but also the use of recommended coprescribed medications for patients with diabetes, such as angiotensin-converting enzyme inhibitors, angiotensin receptor blocking agents, or aspirin.78-80 Payment methods that reward quality of care compared with fee-for-service are helping to overcome some of the financial barriers in addressing SDH.81
Pharmacists can address SDH for older adults in various ways depending on the setting. In the long term-care setting, pharmacists are involved in drug regimen reviews and are on the interdisciplinary team where they can individualize care of the resident.82 Within the healthcare setting, pharmacists can advocate for the adoption of age-friendly health systems, which align with the 4Ms—understanding what matters most to patients in terms of health goals and care preferences; preventing, identifying, treating, and managing conditions which affect mentation, such as dementia, depression, and delirium; ensuring that older adults have safe mobility to maintain function and what matters to them; and choosing medications that are age-friendly and don’t interfere with what matters, mentation, or mobility.83 By performing medication therapy management, pharmacists can ensure that these goals are achieved for their older adult patients.
With so many different medication-administration options, the pharmacist can work with the team and the patient to find the one that the patient is most comfortable with and is covered by their insurance.84-86 Digital health offers another opportunity for pharmacists to engage patients with diabetes by advising on affordable mobile apps that can increase adherence to diabetes self-management as well as smart sensors that provide more accurate glucose measurements.87
Lastly, besides efforts to address gaps in therapy, pharmacists can also play an active role in helping to deprescribe medications. The Choosing Wisely initiative has identified areas involving drug therapy for patients with diabetes in which open dialogue is recommended in order to avoid unnecessary or harmful effects.88 These include discouraging the use of sliding scale insulin for long-term diabetes management among nursing home residents; avoiding medications other than metformin to achieve an HbA1C less than 7.5% in most older adults; and avoiding the use of nonsteroidal anti-inflammatory agents in patients with hypertension, heart failure, or chronic kidney disease, including diabetic nephropathy.
SDH TOOLKIT
A resource that may be useful for pharmacists as they explore the role of SDH in the care of their patients with chronic diseases, including diabetes, is the Community Links Evidence to Action Research Collaboration Toolkit (CLEAR). This toolkit was the result of international efforts spearheaded by the Canadian government to help health professionals better support disadvantaged patients and to promote action on broader social determinants in their local context. It provides contextualized guidance about how to screen for and address SDH.43 The CLEAR toolkit, which is available free of charge in over 10 languages, can be found at www.mcgill.ca/clear/download#English. Pharmacists can employ this tool in their practice settings, such as in pharmacist-led clinics, to help address SDH.
CONCLUSION
As the number of persons with diabetes is projected to markedly increase in the coming years, pharmacists can use a population-based approach that focuses on SDH to address diabetes-management issues that are most important to their patients’ physical and mental well-being. Pharmacists are an integral part of the patient-care team and by working with other members of the team (e.g., physicians, nurses, case managers, social workers, dieticians, psychologists, physical and occupational therapists) they can assist in the management and incorporation of SDH into patient-care plans and treatment regimens. In fact, working as part of a care team is key to a pharmacist’s success in managing and incorporating SDH into patient care. It is important for pharmacists to be able to identify factors that either negatively or positively influence their patient’s ability to engage in healthy choices that can affect their glycemic control. These strategies are especially important to implement during the COVID-19 pandemic. Personalization of care can lead to optimization of drug regimens and increased adherence, which may lead to better outcomes.
REFERENCES
1. CDC. What is population health? www.cdc.gov/pophealthtraining/ whatis.html. Accessed April 5, 2020.
2. U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020. Social Determinants of Health. www.healthypeople.gov/2020/topics-objectives/topic/ social-determinants-of-health. Accessed March 7, 2020.
3. U.S. Department of Health and Human Services. Join us for the Healthy People 2030 launch. https://health.gov/news/202007/join-us-healthy-people2030-launch#:~:text=On%20August%2018%2C%20the%20 U.S.,latest%20iteration%20of%20Healthy%20People! Accessed September 1, 2020.
4. U.S. Department of Health and Human Services. Healthy People 2030: Diabetes. www.healthypeople.gov/2020/topics-objectives/topic/diabetes. Accessed September 1, 2020.
5. CDC. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2020.
6. Lin J, Thompson TJ, Cheng YJ et al. Projection of the future diabetes burden in the United States through 2060. Popul Health Metrics. 2018;16(9).
7. CDC. National Center for Health Statistics. Diabetes. www.cdc.gov/ nchs/fastats/diabetes.htm. Accessed April 5, 2020.
8. U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020. Diabetes. https://www.healthypeople.gov/2020/topics-objectives/topic/diabetes/ objectives. Accessed March 7, 2020.
9. Hill KE, Gleadle JM, Pulvirenti M, et al. The social determinants of health for people with type 1 diabetes that progress to end-stage renal disease. Health Expect. 2015;18(6):2513-2521.
10. Walker RJ, Smalls BL, Campbell JA, et al. Impact of social determinants of health on outcomes for type 2 diabetes: a systematic review. Endocrine. 2014;47(1):29-48.
11. Cranor CW, Bunting BA, Christensen DB. The Asheville Project: long-term clinical and economic outcomes of a community pharmacy diabetes care program. J Am Pharm Assoc (Wash). 2003;43(2):173-184.
12. CDC. National Center for Chronic Disease Prevention and Health Promotion. Rx for the National Diabetes Prevention Program. Action guide for community pharmacists. www.cdc.gov/diabetes/prevention/pdf/ pharmacists-guide.pdf. Accessed March 2, 2020.
13. American Diabetes Association. Improving care and promoting health in populations: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S7-S13.
14. Powers MA, Bardsley JK, Cypress M, et al. Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the American Diabetes Association, the Association of Diabetes Care and Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care. 2020; 43(7):1636-1649.
15. Miles DRB. Brief commentary: social determinants of health and treatment targets for type 2 diabetes. Ann Intern Med. 2018;169(4):252.
16. Tsasis P, Wu J, An A, et al. Conceptualizing type 2 diabetes and its management. J Multidiscip Healthc. 2016;9:133-136.
17. Artiga S, Hinton G. Issue Brief—Beyond health care: the role of social determinants in promoting health and health equity. http://files.kff. org/attachment/issue-brief-beyond-health-care. Accessed April 15, 2020.
18. Herkert D, Vijayakumar P, Luo J, et al. Cost-related insulin underuse among patients with diabetes. JAMA Intern Med. 2019;179(1):112–114.
19. Fiore K, Wickline Wallan S, Chu E. Price tag on old insulin skyrockets. Medpage Today. www.medpagetoday.org/special-reports/specialreports/47603. Accessed March 5, 2020.
20. American Diabetes Association/Vault. Insulin affordability survey, 2018. http://main.diabetes.org/dorg/PDFs/2018-insulin-affordability-survey.pdf. Accessed March 14, 2020.
21. Walker RJ, Gebregziabher M, Martin-Harris B, et al. Independent effects of socioeconomic and psychological social determinants of health on self-care and outcomes in type 2 diabetes. Gen Hosp Psychiatry. 2014;36(6):662-668.
22. Walker RJ, Garacci E, Palatnik A, et al. The longitudinal influence of social determinants of health on glycemic control in elderly adults with diabetes. Diabetes Care. 2020;43(4):759-766.
23. American Diabetes Association. New data highlights severe health and economic impact of pandemic on millions living with diabetes. July 29, 2020. www.diabetes.org/newsroom/press-releases/2020/new-datahighlights-severe-health-and-economic-impact-of-pandemic-on-millionsliving-with-diabetes. Accessed August 24, 2020.
24. Linder S, Marko D, Tian Y, et al. A population-based approach to mapping vulnerability to diabetes. Int J Environ Res Public Health. 2018;15(10):2167.
25. Agency for Toxic Substances and Disease Registry. CDC social vulnerability index. https://svi.cdc.gov/. Accessed September 1, 2020.
26. Herrick CJ, Yount BW, Eyler AA. Implications of supermarket access, neighbourhood walkability and poverty rates for diabetes risk in an employee population. Public Health Nutr. 2016;19(11):2040-2048.
27. Lê-Scherban F, Ballester L, Castro JC, et al. Identifying neighborhood characteristics associated with diabetes and hypertension control in an urban African-American population using geo-linked electronic health records. Prev Med Rep. 2019;15:100953.
28. Walker RJ, Strom Williams J, Egede LE. Influence of race, ethnicity and social determinants of health on diabetes outcomes. Am J Med Sci. 2016;351(4):366-373.
29. Maxwell LG, McFarland MS, Baker JW, et al. Evaluation of the impact of a pharmacist-led telehealth clinic on diabetes-related goals of therapy in a veteran population. Pharmacotherapy. 2016;36(3):348-356.
30. Klug C, Bonin K, Bultemeier N, et al. Integrating telehealth technology into a clinical pharmacy telephonic diabetes management program. J Diabetes Sci Technol. 2011;5(5):1238-1245.
31. American Association of Retired Persons. The AARP Network of Age-Friendly States and Communities. www.aarp.org/livable-communities/network-age-friendly-communities. Accessed April 10, 2020.
32. Iheanacho T, Rosenheck R. Prevalence and correlates of diabetes mellitus among homeless veterans nationally in the Veterans Health Administration. J Soc Distress Homelessness. 2016;25(2):53-59.
33. Sease JM, Franklin MA, Gerrald KR. Pharmacist management of patients with diabetes mellitus enrolled in a rural free clinic. Am J Health Syst Pharm. 2013;70(1):43-47.
34. Kalinowski A, Tinker T, Wismer B, et al. Adapting your practice: treatment and recommendations for patients who are homeless with diabetes mellitus. Health Care for the Homeless Clinicians’ Network: Nashville; 2013. https://nhchc.org/wp-content/uploads/2019/08/2013Diabetes Guidelines_FINAL_20130612.pdf. Accessed April 15, 2020.
35. Gaskin DJ, Thorpe RJ Jr, McGinty EE, et al. Disparities in diabetes: the nexus of race, poverty, and place. Am J Public Health. 2014;104(11):2147-2155.
36. Brookings Institution. Time for justice: tackling race inequalities in health and housing. www.brookings.edu/research/time-for-justice-tackling-race-inequalities-in-health-and-housing/. Accessed April 20, 2020.
37. Pearson ER. Diabetes: is there a future for pharmacogenomics guided treatment? Clin Pharmacol Ther. 2019;106(2):329-337.
38. Florez JC. It's not black and white: individualizing metformin treatment in type 2 diabetes. J Clin Endocrinol Metab. 2014;99(9):31253128.
39. Ajith TA. Why are there variations in the responses of glucagon-like peptide-1 agonists among the type 2 diabetic patients?” Curr Clin Pharmacol. 2019;14:247-248.
40. Liu SY, Walter S, Marden J, et al. Genetic vulnerability to diabetes and obesity: does education offset the risk?. Soc Sci Med. 2015;127:150158.
41. Protheroe J, Rowlands G, Bartlam B, Levin-Zamir D. Health literacy, diabetes prevention, and self-management. J Diabetes Res. 2017;2017:1298315.
42. Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475-482.
43. Frier A, Devine S, Barnett F, et al. Utilising clinical settings to identify and respond to the social determinants of health of individuals with type 2 diabetes—a review of the literature. Health Soc Care Community. 2020;28(4):1119-1133.
44. Ochieng JM, Crist JD. Social determinants of health and health care delivery: African American women’s T2DM self-management. Clin Nurs Res. April 2, 2020. Epub ahead of print.
45. Kim S, Love F, Quistberg DA, Shea JA. Association of health literacy with self-management behavior in patients with diabetes. Diabetes Care. 2004;27(12):2980-2982.
46. Rothman R, Malone R, Bryant B, et al. The relationship between literacy and glycemic control in a diabetes disease-management program. Diabetes Educ. 2004;30(2):263-273.
47. Immunization Action Coalition. Vaccinations for adults with diabetes. https://www.immunize.org/catg.d/p4043.pdf. Accessed March 10, 2020.
48. CDC. Health literacy—find training. www.cdc.gov/healthliteracy/ gettraining.html. Accessed March 31. 2020.
49. Ylitalo KR, Meyer MRU, Lanning BA, et al. Simple screening tools to identify limited health literacy in a low-income patient population. Medicine (Baltimore). 2018;97(10):e0110.
50. National Library of Medicine. HealthReach. https://healthreach.nlm. nih.gov/searchresults?keywords=diabetes&btnsearch=Search&author=&l anguage=&format=&user=&records=10. Accessed September 1, 2020.
51. U.S. Department of Health and Human Services. National CLAS Standards. https://thinkculturalhealth.hhs.gov/clas. Accessed September 1, 2020.
52. Johnson LC, Beach E. The importance of the pharmacist's expanding role on the diabetes team: reinforcing nutritional guidelines for improved glycemic control. Pharm Pract Manag Q. 1997;17(3):32-44.
53. CDC. Diabetes meal planning. www.cdc.gov/diabetes/managing/eatwell/meal-plan-method.html. Accessed April 10, 2020.
54. Lexicomp app. Wolters Klumer. Accessed April 1, 2020.
55. Hess Fischl A, Smith-Marsh D. Type 1 diabetes. www.endocrineweb.com/conditions/type-1-diabetes/type-1-diabetes-treatments. Accessed March 30, 2020
56. CDC. Diabetes. Managing sick days. www.cdc.gov/diabetes/managing/flu-sick-days.html. Accessed April 24, 2020.
57. International Group for Diabetes and Ramadan. BMJ Open Diabetes Research and Care. 2015;3: e000108. Accessed April 20, 2020.
58. Smith JD, Clinard VB. Natural products for the management of type 2 diabetes mellitus and comorbid conditions. J Am Pharm Assoc. (2003). 2014;54(5):e304-e321. Accessed March 5, 2020.
59. Walker RJ, Gebregziabher M, Martin-Harris B, et al. Quantifying direct effects of social determinants of health on glycemic control in adults with type 2 diabetes. Diabetes Technol Ther. 2015;17(2):80-87.
60. Walker RJ, Gebregziabher M, Martin-Harris B, et al. Relationship between social determinants of health and processes and outcomes in adults with type 2 diabetes: validation of a conceptual framework. BMC Endocr Disord. 2014;14:82.
61. Butler AM. Social determinants of health and racial/ethnic disparities in type 2 diabetes in youth. Curr Diab Rep. 2017;17(8):60.
62. Association of Diabetes Care and Education Specialists. Behavioral health and diabetes: practice resources. www.diabeteseducator.org/practice/practice-tools/diabetes-management-tools/mental-health-and-diabetes. Accessed April 4, 2020.
63. Rubino F, Amiel SA, Zimmet P, et al. New-onset diabetes in Covid-
19. N Engl J Med. 2020;383:789-790.
64. Patel MR, Piette JD, Resnicow K, et al. Social determinants of health, cost-related nonadherence, and cost-reducing behaviors among adults with diabetes: findings from the National Health Interview Survey. Med Care. 2016;54(8):796-803.
65. Knight DE, Draeger RW, Heaton PC, Patel NC. Pharmacist screening for depression among patients with diabetes in an urban primary care setting. J Am Pharm Assoc. (2003). 2008;48(4):518-521.
66. Ragland D, Payakachat N, Hays EB, et al. Depression and diabetes: establishing the pharmacist's role in detecting comorbidity in pregnant women. J Am Pharm Assoc (2003). 2010;50(2):195-199.
67. Lisi DM. Diabetes and the psychiatric patient. US Pharm. 2010;35(11):62-79.
68. Cooper SJ, Reynolds GP, Barnes T et al. BAP guidelines on the management of weight gain, metabolic disturbances and cardiovascular risk associated with psychosis and antipsychotic drug treatment. J Psychopharmacol. 2016;30(8):717-748.
69. Ishida S, Takechi K, Bando H, et al. Development and pharmacistmediated use of tools for monitoring atypical antipsychotic-induced side effects related to blood glucose levels. Pharmacoepidemiol Drug Saf. 2018;27(12):1379-1384.
70. Walker RJ, Smalls BL, Egede LE. Social determinants of health in adults with type 2 diabetes—contribution of mutable and immutable factors. Diabetes Res Clin Pract. 2015;110(2):193-201.
71. Barnsteiner JH. Medication reconciliation. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality; April 2008: Chapter 38. https://www.ncbi.nlm.nih.gov/books/NBK2648/. Accessed March 20, 2020.
72. Joint Commission. Hot topics in health care. Transitions of care: the need for a more effective approach to continuing patient care. www. jointcommission.org/-/media/deprecated-unorganized/imported-assets/tjc/ system-folders/topics-library/hot_topics_transitions_of_carepdf.pdf?db=w eb&hash=CEFB254D5EC36E4FFE30ABB20A5550E0. Accessed April 20, 2020.
73. Wu WC, Taveira TH, Jeffery S, et al. Costs and effectiveness of pharmacist-led group medical visits for type-2 diabetes: A multi-center randomized controlled trial. PLoS One. 2018;13(4):e0195898.
74. Benedict AW, Spence MM, Sie JL, et al. Evaluation of a pharmacistmanaged diabetes program in a primary care setting within an integrated health care system. J Manag Care Spec Pharm. 2018;24(2):114-122.
75. Wang Y, Yeo QQ, Ko Y. Economic evaluations of pharmacist-managed services in people with diabetes mellitus: a systematic review. Diabet Med. 2016;33(4):421-427.
76. Morello CM, Zadvorny EB, Cording MA, et al. Development and clinical outcomes of pharmacist-managed diabetes care clinics. Am J Health Syst Pharm. 2006;63(14):1325-1331.
77. Warrington L, Ayers P, Baldwin AM, et al. Implementation of a pharmacist-led, multidisciplinary diabetes management team. Am J Health Syst Pharm. 2012;69(14):1240-1245.
78. Twigg MJ, Desborough JA, Bhattacharya D, Wright DJ. An audit of prescribing for type 2 diabetes in primary care: optimising the role of the community pharmacist in the primary healthcare team. Prim Health Care Res Dev. 2013;14(3):315-319.
79. Chinthammit C, Harrington A, Wild A, et al. Retrospective review of exceptions for angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker recommendations for a diabetic Medicare population. J Manag Care Spec Pharm. 2019;25(3):358-365.
80. LaMarr B, Valdez C, Driscoll K, Ryan M. Influence of pharmacist intervention on prescribing of angiotensin-converting-enzyme inhibitors, angiotensin II-receptor blockers, and aspirin for diabetic patients. Am J Health Syst Pharm. 2010;67(4):290-294.
81. Saulsberry L, Peek M. Financing diabetes care in the U.S. health system: payment innovations for addressing the medical and social determinants of health. Curr Diab Rep. 2019;19(11):136.
82. Centers for Medicare and Medicaid Services. State operations manual. Appendix PP. Guidance to surveyors for long-term care facilities. Revised 173, November 22, 2017. www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_pp_guidelines_ltcf.pdf. Accessed March 20, 2020.
83. Fulmer T. Discovering for 4Ms: a framework for creating an agefriendly health systems. www.johnahartford.org/blog/view/discoveringthe-4ms-a-framework-for-creating-age-friendly-health-systems/. Accessed April 20, 2020.
84. American Association of Diabetes Educations. Strategies for insulin injection therapy for diabetes self-management. www.diabeteseducator. org/docs/default-source/legacy-docs/_resources/pdf/research/aade_meded. pdf?sfvrsn=2. Accessed April 20, 2020.
85. Wahowiak L. Injection aids. Consumer guide 2018. Diabetes forecast. http://main.diabetes.org/dforg/pdfs/2018/2018-cg-injection-aids.pdf. Accessed April 20, 2020.
86. Kubus C, Wick JY. Drug-device combinations: are they appropriate for the aging population? Consult Pharm. 2016;31(5):240-250.
87. Kerr D, King F, Klonoff DC. Digital health interventions for diabetes: everything to gain and nothing to lose. Diabetes Spectr. 2019;32(3):226230.
88. American Board of Internal Medicine Foundation. Choosing Wisely initiative. https://www.choosingwisely.org. Accessed April 20, 2020.