Screening for Depression in Patients With Breast Cancer
RELEASE DATE
October 1, 2022
EXPIRATION DATE
October 30, 2024
FACULTY
Donna M. Lisi, PharmD, BCPS, BCPP, BCGP, BCACP, BCMTMS
Clinical Pharmacist
Somerset, New Jersey
FACULTY DISCLOSURE STATEMENTS
Dr. Lisi has no actual or potential conflicts of interest in relation to this activity.
Postgraduate Healthcare Education, LLC does not view the existence of relationships as an implication of bias or that the value of the material is decreased. The content of the activity was planned to be balanced, objective, and scientifically rigorous. Occasionally, authors may express opinions that represent their own viewpoint. Conclusions drawn by participants should be derived from objective analysis of scientific data.
ACCREDITATION STATEMENT
 Pharmacy
Pharmacy
Postgraduate Healthcare Education, LLC is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education.
UAN: 0430-0000-22-124-H01-P
Credits: 2.0 hours (0.20 ceu)
Type of Activity: Knowledge
TARGET AUDIENCE
This accredited activity is targeted to pharmacists. Estimated time to complete this activity is 120 minutes.
Exam processing and other inquiries to:
CE Customer Service: (800) 825-4696 or cecustomerservice@powerpak.com
DISCLAIMER
Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patients’ conditions and possible contraindications or dangers in use, review of any applicable manufacturer’s product information, and comparison with recommendations of other authorities.
GOAL
To educate pharmacists about depression as a common comorbidity in women with breast cancer and the role that pharmacists can play in the identification, screening, and referral of the mood disorder.
OBJECTIVES
After completing this activity, the participant should be able to:
- Describe the prevalence of depression among women with breast cancer.
- Identify specific challenges due to the COVID-19 pandemic restrictions and obstacles faced by young women with breast cancer.
- Summarize the pharmacogenomic issues surrounding the use of antidepressants in women with breast cancer who are receiving tamoxifen.
- Discuss the role that pharmacists can play in screening women with breast cancer for depression, educating them about available resources, and providing appropriate referrals.
ABSTRACT: Approximately one in eight women will develop breast cancer (BC) in her lifetime, and depression and suicide are higher in this group than in the general population. The necessary COVID-19 pandemic social restrictions resulted in delays in treatment and heightened fears of BC recurrence and disease progression. Young women are particularly vulnerable to depression and face additional challenges compared with older women with BC. Information about the potential gene-drug interaction between tamoxifen (a selective estrogen receptor modulator, which is one of the mainstays of adjunctive hormonal therapy for BC) and some selective serotonin reuptake inhibitors is available. Pharmacists should be actively involved in screening patients with BC for depression, informing them about resources that are available, and making referrals to other team members as appropriate.
In the United States, breast cancer (BC) is the most common type of cancer in women (except for some types of skin cancer), accounting for 30% of all cancers diagnosed in this group.1,2 In 2022, it is estimated that there will be 290,560 new cases of BC in the U.S., along with 43,780 deaths.3 According to the National Cancer Institute (NCI), in 2019 there were an estimated 3,771,794 women living with BC in the U.S.4 BC accounts for 15% of all new cancer cases and 7.1% of cancer deaths among women, with black women dying from the disease at a higher rate than white women.4,5
In the U.S., approximately one in eight women will develop BC in her lifetime, with many suffering from concomitant depression.6
Statistics on Depression and BC
Global estimates put the prevalence of depression among BC survivors at nearly 32.2%.7 One of the most comprehensive studies was a serial, retrospective, crosssectional analysis conducted between January 1, 2002, and December 31, 2014, using data from the Healthcare Cost and Utilization Project National Inpatient Sample, which is the largest all-payer inpatient discharge database in the U.S. This study characterized the type and number of comorbidities with depression in both female and male patients with BC. Among patients hospitalized with BC, 41% of women had metastatic disease, compared with 46% of men. The prevalence of depression was 10.5% among women and 7.5% among men. Comorbidities were more common in men than women. Among hospitalized women with BC, depression was most common in whites and those aged 40 to 69 years, whereas in men, it was more common in Native Americans, Hispanics, and those aged 18 to 49 years.
The investigators also noticed a shift in the prevalence of depression, with rates increasing from 6.5% in non-metastatic disease and 5.9% for metastatic disease in women in 2002 to 15.7% to 14.8%, respectively, in 2014. This represents an increase in diagnosed depression of 6% per year in women. For men, the prevalence of depression was 4.7% for nonmetastatic disease and 4.6% for metastatic disease in 2002, and this increased to 13.8% to 9.8%, respectively, in 2014: a 10% increase per year during that period.8
Several studies have attempted to quantify rates of depression in various populations with BC. In a study of Medicare beneficiaries, depression rates varied based on type of malignancy, with 3.9% of women with BC diagnosed with depression compared with 5.8% of women with colorectal cancer.9 However, another study found that depression was most often identified in patients with BC compared with the other cancer types, including colorectal cancer (27.4% vs. 18.6%, respectively). They also found that the incidence of depression has increased among patients with late-stage cancer of any type from 15.3% in 2001 to 24.1% in 2013. Although not specific for BC, the highest incident of postdiagnosis depression was in whites, and the lowest incidence was among Hispanics. In general, depression was significantly more common in women versus men (22.7% vs. 16.3%, respectively).10 The prevalence of depressive symptomatology was 53% in a group of Latina BC survivors.11
Assessment of Depressive Symptoms in Cancer Patients
More emphasis has been placed on the mental health well-being of cancer survivors in recent years. While not specific for BC, the American Society of Clinical Oncology (ASCO) has recommendations for the screening, assessment, and care of depressive symptoms in adults with cancer (see TABLE 1).12
The NCI has developed a Physician Data Query (PDQ), which is a monograph-like document to assist with the management of depression in patients with cancer. While also not specific to BC, it does address BC throughout. It covers an overview; assessment and diagnosis; intervention for depression in cancer; and the prevalence, assessment, and management of suicide risk in cancer patients.13
The National Comprehensive Cancer Network (NCCN) has developed a Distress Thermometer to screen for distress and rate it on a scale of 0 to 10. Distress is described as an unpleasant experience of mental, physical, social, or spiritual nature. There is also an accompanying Problem List that asks about problems in five different life domains: practical (e.g., childcare, food, housing, insurance/financial, transportation, work/ school, and treatment decisions); family problems; emotional problems; spiritual/religious concerns; and physical problems.14 A PDF of the NCCN Distress Thermometer and Problem List can be found at www.nccn.org.
Healthy People 2030 has added a research objective intended to increase the mental and physical health–related quality of life of cancer survivors (C-R01). Although there are currently no evidence-based interventions available to address this objective, it has been deemed a high-priority public health issue.15
Impact of Depression on Health Outcomes in BC
Depression may adversely affect the immune system.16 Stress may increase susceptibility to inflammationinduced depressive symptoms. Increased levels of inflammation have been associated with increased depressive symptoms in BC.17,18 A systematic review and meta-analysis of cohort studies found that psychological distress, which manifests as depression and anxiety, was associated with higher cancer-specific mortality risk in patients with BC.19 A review of data from 145,251 BC patients from the Korean National Health Insurance Service who were diagnosed between 2007 and 2014 found that depression and/or anxiety significantly increased the risk of mortality (hazard ratio [HR]: depression 1.26, anxiety 1.14, depression and anxiety 1.38, respectively). However, antidepressant therapy attenuated this risk.20 Another study using data from the Taiwan National Health Insurance Research Database for 30,659 newly diagnosed BC patients found that depression was associated with a higher rate of recurrence compared with a nondepressed cohort (17.1% vs. 12.5%, respectively; P <.001).21
There may be a bidirectional relationship between depression and BC that acts via the immune system. One theory is that depression is due to dysfunction of immune cells and cytokines resulting from alterations to neurotransmitters (including serotonin) that affect blood-brain permeability. There may also be alterations in tryptophan metabolism. A common link may exist between the dysregulation of cytokines or the gastric microbiota, depression, and BC.22 Among the cytokines that have been found to be linked to depression in BC patients are interleukin (IL)-8, IL-6, and IL-2.23-26 Stress in the form of social environmental adversity (e.g., crime, adverse childhood experiences) is related to depression and anxiety symptoms, which may increase risk by acting as potential modulators of the tumor microenvironment in BC.27,28 BC itself may serve as a “second wave” of stress, which could affect the development and progression of BC through the hypothalamicpituitary axis.29 Increased psychosocial resilience may help mitigate inflammation-caused depression in BC.30
Depression has also been shown to be directly correlated to pain severity and interference in function among BC survivors.31 It may also be involved in chemotherapy-induced memory problems.32 Higher depression scores are associated with worse sleep quality.33 Having depression prior to a BC diagnosis may affect treatment options and thereby impact prognosis.34
The Total Beck Depression Inventory score may serve as a useful tool to predict 25-year relapse-free survival and overall survival in BC patients.35
Despite the prevailing evidence linking depression to the risk of BC, a meta-analysis involving 11 cohort studies and 182,241 participants concluded that there are insufficient data to support a positive association between depression and BC. It cited methodological concerns, including the use of single depression assessments and numerous different depression scales.36
COVID-19 Effects on Psychosocial Well-Being and BC Treatment Delays
The COVID-19 pandemic and initial mandatory social restrictions have had an adverse effect on the psychosocial well-being of the general population, but more specifically on patients with cancer.37 In an observational longitudinal study of patients undergoing IV antineoplastic therapy, patients with BC experienced greater COVID-19 distress compared with those with other types of cancer (i.e., lung, gastrointestinal, genitourinary, nervous system, head and neck, melanoma, other gynecological cancers, and sarcoma); BC patients made up 26% of the study population.38 The pandemic lockdown restrictions also led to disruptions of care for about one-half of BC survivors.39 Significantly more patients with depression experienced barriers in contacting their general practitioner and BC physician (25.0% and 11.2%, respectively). Interruption of treatment or after-care plans were significantly correlated with depression in one-third (32.7%) of patients. Previously having had depression was independently and significantly associated with depression during the pandemic.40
Another study also found that being unable to contact the physician during the pandemic was associated with deterioration in BC patients’ emotional functioning. In those undergoing active BC treatment, there was a significant decline in social functioning during the pandemic. About one-half reported moderate-to-severe loneliness.41 In a study of older BC survivors, loneliness increased during the pandemic in both patients with BC and those without BC. The loneliness was not explained by either the older adults’ living situation or the availability of a support system. In both groups, loneliness was associated with worsening mental health.42
Depression and anxiety increased death anxiety among BC survivors during the pandemic.43 A scoping review of fear of BC recurrence during the pandemic found that 35.7% of BC patients experienced a clinically significant level of fear. Risk factors for increased fear of BC recurrence were being unmarried, childless, and less financially secure.44 This fear may be justified as another study found that there was a significant increase in the prevalence of BC recurrence among those whose treatment was delayed due to COVID-19 restrictions compared with those whose care was not delayed (18.4% vs. 9.0%, P = .018).45
For patients with BC, the lockdown had an additional impact of limited access to timely and muchneeded healthcare. Treatment changes, which affected one-fifth of patients (18.8%), and changes in treatment plans due to the pandemic were significantly associated with depression.46
A survey was conducted from April 2020 to May 2020 (the first lockdown) of 201 women with BC (median age 53.12 years) who were awaiting treatment at an infusion center. About 47% had been diagnosed with BC more than a year prior. Researchers found that over one-half (54.2%) of patients experienced high distress as indicated by the NCCN’s Distress Thermometer and Problem List. Among the issues that were associated with a high level of distress were those involving childcare, housing, or work or school, and having depression, feeling fear, nervousness, sadness, worry, loss of interest for usual activities, sleep problems, and difficulty getting around. Those diagnosed more than 12 months prior most often had the highest level of distress (25.9% for those diagnosed more than 12 months ago, 13.4% for those diagnosed 6 to 12 months prior, and 14.9% for those diagnosed less than 6 months ago).47
A study from Canada found that 63.9% of BC patients experienced at least one stressor during the pandemic. Stressors with the highest degree of concern included obtaining food, medicine, and essentials; postponement or cancellation of cancer treatment; changes in cancer-care trajectory; and postponement of medical tests. The higher the number of stressors and the greater the level of concern, the more significant was the association with depression.48
Among the protective factors associated with reduced depression, anxiety, and stress during the lockdown were the possession of personal positive resources such as optimism, hope, self-efficacy (i.e., the belief of being able to perform new or difficult tasks and to achieve the desired results), trait mindfulness (i.e., the predisposition to be mindful in day-to-day life), and courage.49
Conversely, a study from the UK that evaluated the impact of COVID-19 on psychological distress among cancer patients (BC patients made up 58.6% of the patient population in 2019 and 41.3% in 2020) found that the pandemic did not adversely affect mental health.50 Another group found similar results but also identified a subgroup of BC patients undergoing active treatment who were psychologically susceptible to high levels of distress and lower quality of life due to their “concern often/all the time” about COVID-19.51
Physical and Psychological Effects of BC in Young Women
Young women with BC face unique physical and psychological challenges, such as infertility/trying to preserve fertility, child-rearing and fear of leaving their children motherless, interference with career trajectory, sexual functioning, financial concerns, and social isolation.52-57 Factors that add to distress in young women with BC include that the disease is more likely to be hereditary, may be found at a later stage, and may be more aggressive.57 Studies that have focused on BC in young women have used different age cutoffs to define this population, ranging from age 18 to 50 or 55 years, adding difficulty in assessing the effect of depression in this group.
In the U.S., about 9% of all new BC cases are diagnosed in women younger than age 45 years.57 Whereas the incidence of BC has decreased in older women, recent statistics from the CDC show that the incidence has increased for women aged 20 to 39 years.2
Rates of depression in young women with BC range from 18% to 43%, are higher compared with rates in older women (age >50 years), and are more elevated than in the general population.58,59 Rates of anxiety symptoms are even higher, occurring in up to 69% of young women.58,60 Others have confirmed that anxiety, rather than depression, appears to be more common in this population.61 Some studies have found that depression and anxiety symptoms are at their highest early on in the course of disease, especially when first diagnosed and while undergoing treatment.62 Others have indicated that quality of life and psychological distress, including depression, are dynamic over the first year following surgery in young women. Monitoring of psychosocial status should be ongoing.61 In a study of 54 young women with metastatic BC, investigators found that 20% of patients had a positive screen for depression and 44% had a positive screen for anxiety.63
Concerns over fertility are one of the major sources of distress in young women with BC.52,54 This is especially true for women who are nulliparous at the time of treatment and for whom treatment results in ovarian failure.54 It has been recommended that premenopausal women receiving systemic therapy and who desire to have children consult a reproductive endocrinologist prior to treatment to determine fertility-prevention strategies. Hormonal therapy is not recommended.64,65 Several recent studies offer reassurance that fertility preservation is safe.66-68
Young women with chemotherapy-induced infertility score lower in assessments of health-related quality of life and physical functioning than do noncancer patients suffering from infertility.69 The Young and Strong study was a multisite, cluster-randomized clinical trial to address fertility concerns. These concerns then served as a surrogate marker for other issues faced by young women with BC. The trial also sought to educate and provide support and reduce psychosocial distress that accompanies a BC diagnosis.70 However, the program was not successful in bringing attention to fertility issues.71 Others have found that an interventional strategy such as a fertility-related decision aid designed to educate young women about fertility-related options helped reduce distress and later regrets.72
A systematic review of health-related quality of life, menopausal symptoms, and fertility concerns among women aged younger than 50 years with BC found that premature menopause, menopausal symptoms, and infertility following treatment were associated with higher levels of distress.59 Menopausal symptoms, in particular vasomotor symptoms, appear to mediate depression by causing sleep disturbances. Use of nonhormonal pharmacologic agents such as antidepressants, gabapentin, or nonpharmacological interventions (e.g., cognitive behavioral therapy) may help relieve vasomotor symptoms and the associated depression.73 Additionally, chemotherapy-induced menopause has been associated with both sexual inactivity and sexual dysfunction in young women with BC.55
Risk factors for depression in young BC survivors include the presence of preexisting depression, having children aged younger than 10 years, and having an income above $100,000.58 A prior diagnosis of depression has been associated with reduced family support.74 Family and partner support, body image, and the ability to manage children and daily life in general also play a mediating role in depression and/or anxiety.56,74,75 In a systematic review in young BC survivors, emotional support and self-esteem were negatively associated with depressive symptoms, whereas illness intrusiveness into daily activities, stress, negative body image, pain, reproductive concerns, and poor physical functioning were positively associated with depressive symptoms.59 Data from the Young and Strong trial of BC survivors found that income was not associated with a diagnosis of depression.76 In young women with metastatic BC, having a college education, a higher physical symptom score, being white, having less social support, and having lower spirituality were associated with higher depression scores.63
The type of surgical procedure (i.e., mastectomy or breast-conserving surgery [lumpectomy]) also affects the level of distress.77 Young women who underwent a bilateral mastectomy experienced more sexual and body image distress than those who underwent breast conservation, especially if the mastectomy was not followed by reconstructive surgery.77,78
Mindfulness meditation and survivorship education have been shown to reduce symptoms of depression. Mindfulness has been associated with additional benefits in relieving fatigue, insomnia, and vasomotor symptoms.79 Psychological resilience improves outcomes.80 Increasing physical activity and healthy eating may also improve mood in young women with BC.81
Partners of young survivors are adversely affected by the BC diagnosis.82 There appears to be a bidirectional relationship with each partner affected by each other’s level of distress.83
Priority research areas that have been identified for young women with BC include promoting shared decision-making, addressing concerns over body image, fear of recurrence and treatment, and evaluating palliative care options for patients with metastatic disease.62
Guidelines on Tamoxifen and Drug-Drug Antidepressant Interactions
Tamoxifen is one of the mainstays of adjunctive hormonal therapy in BC. Tamoxifen is extensively metabolized by numerous CYP450 enzymes, including CYP3A, CYP2D6, CYP2C9, CYP2C19, and CYP2B6. N-desmethyltamoxifen, which is tamoxifen’s major metabolite with equipotent activity to tamoxifen, is primarily formed by CYP3A. Although considered minor metabolites, endoxifen and 4-hydroxytamoxifen have 100fold greater affinity for the estrogen receptor and 30- to 100-fold greater potency in suppressing estrogen-dependent cell proliferation than tamoxifen.
CYP2D6, which undergoes polymorphism resulting in various metabolizer states (i.e., poor metabolizer [PM], intermittent metabolizer [IM], and ultrarapid metabolizer [UM] status), is involved in the formation of endoxifen and 4-hydroxytamoxifen. CYP2D is responsible for catalyzing the formation of endoxifen from N-desmethyltamoxifen. Phase 2 enzymes, such as SULT1A1, UGT2B7, and UGT1A4, are associated with tamoxifen clearance from plasma.84
The ABCB1 transporter, which is also subject to polymorphism, is thought to play a role in the metabolism of tamoxifen. The ABCB1 gene encodes for p-glycoprotein, an efflux transporter that extrudes drug molecules and xenobiotics at the blood-brain barrier (BBB) level. The wildtype of the ABCB1 transporter increases efflux of substrate antidepressants at the BBB. ABCB1 genotype has been linked to antidepressant treatment response.85 ABCB1 polymorphisms may affect the outcome of tamoxifen adjuvant treatment in premenopausal BC patients86-89
The Clinical Pharmacogenetics Implementation Consortium (CPIC) developed guidelines to address the effect of CYP2D6 polymorphism on tamoxifen’s metabolism.90,91 Metabolism of N-desmethyltamoxifen to endoxifen via CYP2D6 varies depending on phenotype. Low endoxifen concentrations have been associated with an increased risk of BC recurrence in women who are on tamoxifen as adjunctive therapy for BC. However, the use of CYP2D6 metabolizer phenotype as a predictor of clinical outcome is controversial.92,93 There is no established “lower limit” of circulating endoxifen that is associated with treatment failure. Only low levels of endoxifen are needed to block all receptors. Even when alterations in CYP2D6 metabolizer status have occurred resulting in shorter time to recurrence and poorer relapse-free survival, there have been no observed differences in overall survival. However, the studies used to draw this conclusion have been criticized for being flawed.94
A systematic review and meta-analysis on the CYP2D6 genotype and tamoxifen response for BC published in 2013 that included 25 studies and 13,629 patients concluded that despite a weak association between CYP2D6 genotype and surrogate endpoints for overall survival, the use of CYP2D6 genotyping to guide tamoxifen prescribing is not recommended.95 More recently, in April 2022 another systematic review involving 15 studies came to a similar conclusion that despite data from nearly 100,000 patients on tamoxifen and selective serotonin reuptake inhibitor (SSRI) therapy, including paroxetine, there is no consistent evidence of harm (i.e., BC-specific survival, mortality, quality of life, treatment compliance, and impact of concurrent use of antidepressants and other endocrine therapies) from concomitant use. The authors questioned whether it was time to update evidence-based guidelines to reflect this conclusion.96 However, caution is advised since one study demonstrated statistically significant evidence of adverse effects on mortality (HR 1.36, 95% CI 1.15-1.61) included in the systemic review.
The CPIC guidelines make recommendations on the use of endocrine therapy based on CYP2D6 phenotype. CYP2D6 PMs (i.e., those who have deficit CYP2D6 activity) have lower endoxifen concentrations compared with normal (extensive) metabolizers. Since this can increase the risk of BC recurrence, aromatase inhibitors (AIs; e.g., anastrozole, letrozole, exemestane) are recommended alternatives for postmenopausal women. For premenopausal women who are PMs, the guidelines recommend the use of AIs along with ovarian-function suppression. Switching from tamoxifen to anastrozole is not associated with an increased risk of BC recurrence. The guidelines do not recommend the use of a higher dose of tamoxifen (i.e., 40 mg/day) unless AIs are contraindicated because this dosage does not normalize endoxifen concentrations. In patients who are IMs or IMs/normal metabolizers, AIs are also recommended with or without ovarian suppression based on menopausal status, and the 40-mg/day dosage of tamoxifen should only be used if AIs are contraindicated. Patients should also avoid CYP2D6 inhibitors of any type (weak or strong inhibitors). Normal and ultra CYP2D6 metabolizers (i.e., those with genetically elevated CYP2D6 activity) should receive the recommended standard dosage of tamoxifen (20 mg/day), but they should avoid moderate-to-strong CYP2D6 inhibitors.90,91 Evidence shows that there has been a shift in prescribing patterns away from the concomitant use of strong CYP2D6-inhibitory antidepressants with tamoxifen.97,98
Concern arises in the management of depression in patients with BC since several antidepressants are CYP2D6 inhibitors. Paroxetine, fluoxetine, and bupropion are strong inhibitors; duloxetine is a moderate inhibitor; and escitalopram, citalopram, venlafaxine, sertraline, fluvoxamine, and mirtazapine are weak inhibitors of CYP2D6, with the latter two presumably having no CYPD2D6 activity.99,100 Those who are CYP2D6 PMs already have higher concentrations of drugs such as paroxetine since the antidepressant is also metabolized via CYP2D6, which could lead to greater CYP2D6 inhibition of endotoxifen concentrations.101,102
While paroxetine reduces tamoxifen’s active metabolite, endoxifen, the use of citalopram with tamoxifen has not been associated with BC recurrence (compared with nonusers of citalopram).103-106
Based on results of a population-based cohort study, coadministration of paroxetine and tamoxifen resulted in an increased risk of death from BC (mean follow-up 2.38 years). Absolute risk of BC death increased 25%, 50%, and 75% in proportion to the time on tamoxifen. Overlapping paroxetine administration was associated with 24%, 54%, and 91%, respectively, increased risk of BC-related death.107 However, a large, longitudinal cohort study involving administrative claims data of 16,887 BC survivors found that concomitant administration of tamoxifen and antidepressants, including paroxetine, did not increase the risk of subsequently developing BC over the 14-year study period.108 These findings were confirmed in a case-control study involving 18,432 BC patients with estrogen-positive disease without distant metastases (445 BC patients died due to BC) who were followed for about 10 years. Nonadherence, which was defined as <80% overlap between an SSRI and tamoxifen and was based on data from 9,104 women, was associated with worse BC survival (odds ratio [OR] 4.07, 95% CI 3.27-5.06).109
Some have suggested that continuous SSRI use is associated with lower survival in cancer patients in general (i.e., breast, melanoma, prostate, lung, and colorectal cancers), especially during the first 2 years following a cancer diagnosis.110 Another study based on data from a cancer registry from 1990 to 2008 of 4,216 women with BC did not find that antidepressant use increased the risk of recurrence.111
The FDA has evaluated the scientific evidence for genetic polymorphisms or genetic variant–inferred phenotypes that are likely to affect drug metabolism resulting in either altered efficacy or adverse event profile. For the tamoxifen-CYP2D6 drug-gene interaction pair, the FDA has determined that the pharmacogenetic association demonstrated by the available data results in only a potential impact on pharmacokinetic properties, although it cautions that CYP2D6 IMs or PMs have lower systemic active metabolite concentrations, but the effect on efficacy is not established. The agency has advised the use of caution when this drug-gene pair is present, but the FDA-approved drug label for tamoxifen does not discuss genetic testing for CYP2D6.84,102 This is in contrast to a recommendation based on the scope and strength of evidence by the FDA Clinical Pharmacology Subcommittee in 2006 that supported the inclusion of pharmacogenetic information on CYP2D6 in tamoxifen’s labeling to help improve the benefit/risk ratio of the drug.112,113
CYP2D6 PM status occurs in 3% to 10% of Caucasians, 4.3% to 5.4% of African Americans, 3.8% of South Asians, 0.84% of East Asians, 2.2% to 6.6% of Hispanics, 3.1% of Native Americans, and 2.3% of Middle Easterners.114-116
Pharmacists can play a role by performing pharmacogenomic testing using this information to help guide antidepressant therapy. This is especially important given the potential drug-drug interaction between tamoxifen and SSRIs. Pharmacogenomic-guided antidepressant treatment has been found to result in greater improvement in depressive symptoms, generalized anxiety, and disability compared with standard antidepressant treatment.117 However, pharmacogenomicstudies are needed in patients with depression and BC.
To avoid or minimize CYP2D6 inhibition, safe antidepressants include venlafaxine, desvenlafaxine, mirtazapine, escitalopram, and citalopram.93,105,106,118-120 For patients on tamoxifen and paroxetine or fluoxetine, switching to escitalopram was found to be safe and resulted in threefold higher endoxifen exposure.120 Others have warned that the concomitant use of tamoxifen and SSRIs, in particular paroxetine, escitalopram, and citalopram, has been associated with a significant elevation in the mean QTc-interval, making these latter two drugs less ideal options.121 Any change in the drug regimen of a patient on tamoxifen and a known CYP2D6 inhibitor should be performed gradually to minimize the risk of SSRI withdrawal and idiosyncratic adverse effects.122
Tamoxifen is also metabolized by CYP3A4, which can be induced by St. John’s wort (SJW), resulting in the possible reduction of the selective estrogen receptor modulator’s effectiveness.123 Pharmacists should conduct thorough medication histories to determine whether depressed BC patients are self-medicating with SJW, and they should counsel them to avoid use until further information is available.
On the flip side, there is evidence, albeit it weak, that tamoxifen may be associated with drug-induced depression as tamoxifen crosses the BBB. However, this iatrogenic effect may be a result of confounding since patients with BC are at a higher risk for depression.100,124
Breast Cancer and Suicide: 988 Crisis Hotline
BC survivors are at increased risk of suicidal ideations and completed suicides. Suicide risk appears to be 35% to 53% higher than in the general population.125,126 Unfortunately, there has not been a decrease in the rates of suicide mortality among BC patients for at least 30 years.125 These numbers may be underestimations and may go unrecognized because suicide may take the form of withdrawal of therapy, there may be reluctance to report death by suicide, and there are methodological issues related to the validity of suicide statistics.13,127
Some have reported that the risk of suicide is greatest within the first 3 years following a BC diagnosis, yet others have reported an elevated risk decades later.125,126 It is imperative to identify risk factors for suicide in this population so that prophylactic measures may be implemented.
A retrospective study was performed of data from the Surveillance Epidemiology and End Results (SEER) database of BC patients who committed suicide. Between 1973 and 2013, 474,128 patients with BC were identified as having died from any cause, of which 773 had committed suicide. Investigator found that age (highest risk was in the aged 30-49 years group with an OR 10.64, P <.001, followed by age <30 years, OR 6.34, P = .002, and 50-69 years, OR 4.7, P <.001), male sex (OR 4.34, P <.001), nonwhite, nonblack race (OR 1.39, P = .046), marital status (OR 1.35 for single persons, P = .024 vs. OR 1.25 for those who were separated/divorced/ widowed, P = .043), having undergone cancer-direct surgery (OR 2.13, P = .007), time since BC diagnosis (OR for first year since diagnosis 4.67, P <.001 and OR for second year since diagnosis 2.35, P <.001) and those with progesterone-receptor positive BC (OR 1.74, P = .004) were risk factors for completed suicide.125
Another SEER-based study was published based on data from 2000 to 2014 that involved 4,671,989 patients, of which 1,585 had committed suicide within a year of any cancer diagnosis. When specifically analyzing data on BC, researchers did not observe an increase in suicide risk among those with either localized/regional disease or distant (metastatic) disease.128
In the largest and longest international study to date on suicide among BC survivors, investigators gathered data on 723,810 women reported to 16 populationbased BC registries between January 1, 1953, and December 31, 2001. A total of 836 patients had committed suicide. Risk of suicide was found to remain elevated even 25 years or longer after the BC diagnosis. This risk was slightly but not significantly higher in the initial years following the BC diagnosis. Suicidal risk was highest among black women. Worsening disease (i.e., increasing stage of disease) was also associated with increased risk. The cumulative probabilities of committing suicide following 5, 10, 20, and 30 years since BC diagnosis were 0.05%, 0.10%, 0.16%, and 0.20%, respectively. The authors called for long-term psychosocial follow-up of BC survivors.129
One study of 284 BC survivors found that the prevalence of suicidal ideations was 10.9% 1 week after breast surgery and increased to 11.4% 1 year post surgery. The authors postulated that the mechanisms for short-term and longer term suicide ideations differed. Depression and physical disability were associated early on with depression, but other factors such as living alone, having anxiety, having an advanced stage of disease, and having the brain-derived neurotropic factor (BDNF) promoter methylation allele had more longterm effects.130 Preliminary evidence shows that BDNF gene methylation status may serve as a biomarker for suicidality in BC patients.131
A longitudinal study involving 431 women with stage I to III BC in which patients were surveyed prior to surgery and again at 1 year following surgery found that suicidal ideation had increased from 4.3% at baseline to 12.8% at the year follow-up, respectively. Risk factors for suicidal thoughts included living in the countryside (OR 2.24, P = .027); having a history of traumatic experiences (OR 7.72, P = .01); being employed (OR 2.55, P = .043); and having symptoms of post-traumatic stress disorder (OR 2.89, P = .05). Protective factors against suicidal ideation included patient age of >55 years (OR 0.32, P = .028); having a paid job in recent years (OR 0.34, P = .037); and being satisfied with the way the patient was informed about their disease (OR 0.18, P = .001).132 Chemotherapeutic regimens often include the use of corticosteroids to help manage antineoplastic-induced nausea and vomiting and immune-related adverse effects, for pain relief and appetite stimulation, and to promote a sense of well-being. However, these drugs are also associated with adverse psychological effects, including depression and suicide.133 In addition to corticosteroids, the NCI PDQ identifies other medications associated with contributing to or inducing depression, including endogenous and exogenous cytokines (e.g., interferon-alfa and aldesleukin [IL-2], methyldopa, reserpine [which is no longer available in the U.S.], barbiturates, propranolol, certain antibiotics [e.g., amphotericin B], certain chemotherapeutic agents [e.g., procarbazine, asparaginase], and hormone therapy [e.g., androgen deprivation therapy]).13
Several studies have found that women undergoing reconstructive breast surgery following a mastectomy may be at a greater risk of suicide. The authors advise that psychological evaluation and counseling be performed prior to the procedure.134,135
Upon further analysis of depression as a cause of suicide in BC survivors, it has been suggested that one of the most potent risk factors is hopelessness, which manifests as a negative view of the future, perceived helplessness towards affecting outcomes, and deficits in social problem-solving.16,136 Preliminary evidence has indicated that behavioral activation treatment (BAT) and problem-solving therapy (PST) may reduce depression and suicidal ideation while decreasing hopelessness in BC survivors; these effects may last for at least a year. These forms of psychotherapy are time-limited and teach positive adaptive behaviors.16 BAT increases reinforcement for positive, healthy behaviors by decreasing negative reinforcement and extinguishing maladaptive behaviors.16 PST helps patients with problem identification, efficient problem-solving, and managing associated depressive symptoms.16,137
A study in Denmark that involved 45,325 women diagnosed with primary early-stage BC between 1998 and 2011 found that women who had used antidepressants prior to their diagnosis were less likely to receive guideline-directed BC treatment and were more likely to only receive a biopsy, not surgery. Further, significantly fewer women who had been pharmacologically treated for depression received guideline systematic adjuvant BC therapy. This group had significantly higher cumulative BC-specific mortality compared with women who had not received the psychotropic (13% vs. 11% women had died of BC within 5 years of diagnosis, respectively). Overall survival (HR 1.21, 95% CI 1.14-1.28) was also reduced in the antidepressant-treated group. The risk of suicide was significantly increased for women who used antidepressants (HR 5.38, 95% CI 2.16-13.37) and those who had a previous hospital contact for depression (HR 19.81, 95% CI 5.32-73.86). Although factors for nonadherence to BC treatment guidelines were not discussed, it raises concern about systemic healthcare system bias against those with mental health issues and/or the ability of those suffering from depression to fully participate in their healthcare decisions.138
In September 2020, Congress passed the National Suicide Hotline Designation Act, which required that the Federal Communications Commission (FCC) designate 988 as the universal telephone number for the country’s national suicide prevention and mental health crisis hotline. This legislation was signed into law on October 17, 2020, and went into effect on July 16, 2022.139
The enactment of this law was in response to the grim statistic that in the U.S. there is one death by suicide about every 11 minutes and to the realization that mental health crises are often inappropriately managed through the judicial system instead of the healthcare system.140,141 In addition to the deployment of 988 as the new national hotline number, the legislation also calls for strengthening and expanding the existing crisis network program and providing direct, life-saving services to those in need.142 There are over 200 crisis centers that are part of a national network available to immediately serve the needs of persons in crisis.140
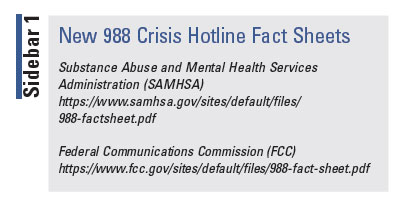 SIDEBAR 1 includes links to patient handouts that
pharmacists can use to educate their patients about the
availability of the new national 988 crisis hotline.
SIDEBAR 1 includes links to patient handouts that
pharmacists can use to educate their patients about the
availability of the new national 988 crisis hotline.
Role of the Pharmacist
Pharmacists can play a major role in screening for depression, in promoting medication adherence, and in suicide prevention for all patients, but especially for those with BC who are at increased risk.143-157 They can help fill the gap in access to mental health services.158,159
The American Pharmacists Association (APhA) Foundation issued a white paper advocating for expanding the role of the community pharmacist in managing depression.160 The APhA Foundation Coordinating Council provided evidence of community pharmacists’ collaborative role in managing patients with depression, and it has advocated that by increasing involvement of community pharmacists in managing patients with depression, pharmacists can improve clinical outcomes and enhance quality of life. Pharmacists can meet the major needs of patients with depression by providing general information about the condition and its treatment; helping patients access appropriate, quality care; providing medication management and support; offering social support and resources; assisting with coordination of care; and increasing pharmacist involvement. The white paper stressed the importance of pharmacistconducted medication therapy management (MTM) reviews.160
Among the screening tools for depression that the white paper recommended were the Patient Health Questionnaire (PHQ)-9 and the PHQ-2.160 Pharmacists should take an active role in identifying patients at risk for depression; screening patients for comorbidities and other risk factors; performing MTM, medication counseling, and education; monitoring medication adherence; participating in collaborative practice agreements; providing information on how patients can access patient pharmaceutical assistance programs; serving as a referral and resource for information about depression and social support resources; and being involved in local/regional/national mental health organizations, advisory boards, and other supportive resources.160
Strategies to enhance pharmacists’ role in managing patients with depression include increasing education about depression in pharmacy school curricula; collaborating with physicians to identify patients at risk; providing patient education; collaborating and communicating with providers; assessing quality of care and patient outcomes; and increasing awareness of the pharmacist’s role and involvement in public and private groups.
Among the actions identified by the Council for ways that community pharmacists can enhance their role in the management of depression are creating and implementing a national stigma-reduction program (e.g., Depression Is Real campaign), creating and implementing interdisciplinary depression-care education and certificate programs for pharmacists and other providers; encouraging screening for depression and incorporating it into MTM: increasing awareness of the pharmacist’s role; developing an organizational value-based design that includes best practices for depression; encouraging pharmacists’ involvement in the implementation and screening of quality measures for depression; and collaborating with other professional and community stakeholder organizations to improve the care of patients with depression.160
The American Society of Health-System Pharmacists (ASHP) issued a policy position statement in 2019 pertaining to the pharmacist’s role in suicide awareness and prevention. It states that pharmacists should be recognized as key providers on the patient care team and that they are integral to suicide awareness and prevention efforts. Potential activities that pharmacists may engage in include ensuring the appropriate use of medications for mental health disorders; identifying and evaluating suicide risk; and making and following up on referrals pertaining to mental health issues. ASHP advocates for mandatory suicide awareness and prevention training for pharmacists and for adequate funding for suicide awareness and prevention efforts.161
The NCI’s PDQ on depression provides screening questions that pharmacists can utilize to assess depressive and suicidal symptoms in patients with cancer.13
Health plans are struggling to collect and use patientreported clinical data for quality measurement. One area that poses a challenge in data collection is the lack of routine depression screening and ongoing assessment.162 The 2023 Centers for Medicare and Medicaid Quality Rating System (QRS) measures address the management of depression. Requirements in 2023 for Antidepressant Medication Management include the percentage of members aged 18 years and older who were treated with antidepressant medication, had a diagnosis of major depression, and remained on an antidepressant medication treatment. Two rates are reported, as follows163:
Effective Acute Phase Treatment: The percentage of members who remained on an antidepressant medication for at least 84 days (12 weeks).
Effective Continuation Phase Treatment: The percentage of members who remained on an antidepressant medication for at least 180 days (6 months).
Pharmacists can assist with these data-collection efforts. One strategy to improve pharmacists’ mental health skills is for them to become Mental Health First Aid (MHFA)–certified. MHFA is a national program to teach the skills to respond to the signs of mental illness (including depression and suicidal ideations) and substance use. MHFA uses the acronym ALGEE, which stands for: Assess risk; Listen nonjudgmentally; Give reassurance and information; Encourage appropriate professional help; and Encourage self-help and other support strategies.164 When pharmacy students underwent MHFA training, it helped to reduce mental health stigma, improve the identification of mental disorders, and improve pharmacists’ confidence in assisting patients with mental health issues.165 Patients have stated that they are more comfortable discussing their mental health issues with a community pharmacist if the pharmacist is MHFA-certified.166
Pursuing board certification in psychiatric pharmacy (BCPP) is another path to increasing knowledge regarding the pharmaceutical care of patients with psychiatric-related illnesses and disorders. Currently, there are more than 1,470 BPS board-certified psychiatric pharmacists.167
While there is a paucity of information on the pharmacist’s role in screening for and managing depression in patients with BC, the literature is replete with evidence of the beneficial effects of screening and referral by pharmacists, including in specific patient populations such as those with cancer (11.7%-15.8% had BC), perinatal women, and patients with diabetes.86,143-150,152-154 Further, pharmacists’ involvement in the collaborative care treatment for depression has resulted in improvement of depression symptoms, adherence, reductions in total healthcare costs, and increased antidepressant prescribing.156,168-171
An important caveat that pharmacists should be aware of is that common assessment tools to screen for depression (i.e., Geriatric Depression Scale–Short Form, the Hospital Anxiety and Depression Scale, and the Center for Epidemiological Studies Depression [CESD] Scale-Revised) may unreliably identify depression in geriatric cancer patients as the established cutoff scores for a positive depression screen may miss 33% to 83% of depressed older patients.172-174 Among these tests, the CESD shows the most utility. Pharmacists should collaborate with their mental health colleagues if questions arise.175
More work and support are needed for the benefit of pharmacists’ involvement in depression screening and referral to be fully realized, as many studies have been small and/or pilot studies. A recent systematic review of depression screening by pharmacists in the community found that while pharmacists are successfully able to screen patients, there is little evidence on the clinical and economic impact of these screenings. The authors called for more well-designed studies.176 These studies should include patients with BC and concomitant depression.
Conclusion
Depression is common in women with BC. Young women with BC are especially at risk for the mood disorder. The use of tamoxifen with strong CYP2D6 inhibitors such as paroxetine and fluoxetine should be avoided. Pharmacists can play a major role in screening BC patients for depression, identifying those at risk for suicide, and making appropriate referrals for follow-up care.
REFERENCES
1. American Cancer Society. Cancer facts for women. https://www.cancer.org/healthy/cancer-facts/cancer-facts-for-women.html#:~:text=Breast%20cancer%20is%20the%20most,up%20as%20you%20get%20older. Accessed July 15, 2022.
2. Ellington TD, Miller JW, Henley SJ, et al. Trends in breast cancer incidence, by race, ethnicity, and age among women aged ≥20 years — United States, 1999–2018. MMWR Morb Mortal Wkly Rep. 2022;71:43-47.
3. American Cancer Society. Cancer Statistics Center. 2022 Statistics. https://cancerstatisticscenter.cancer.org/#!/. Accessed July 15, 2022.
4. National Cancer Institute. Cancer stat facts: female breast cancer. https://seer.cancer.gov/statfacts/html/breast.html. Accessed July 15, 2022.
5. U.S. Centers for Disease Control and Prevention. Breast cancer statistics. https://www.cdc.gov/cancer/breast/statistics/index.htm. Accessed July 15, 2022.
6. American Cancer Society. Key statistics for breast cancer. https://www.cancer.org/cancer/breast-cancer/about/how-common-is-breast-cancer.html. Accessed July 15, 2022.
7. Pilevarzadeh M, Amirshahi M, Afsargharehbagh R, et al. Global prevalence of depression among breast cancer patients: a systematic review and meta-analysis. Breast Cancer Res Treat. 2019;176(3):519-533.
8. Zoorob RJ, Salemi JL, Mejia de Grubb MC, et al. A nationwide study of breast cancer, depression, and multimorbidity among hospitalized women and men in the United States. Breast Cancer Res Treat. 2019;174(1):237-248.
9. Alwhaibi M, Sambamoorthi U, Madhavan S, et al. Cancer type and risk of newly diagnosed depression among elderly Medicare beneficiaries with incident breast, colorectal, and prostate cancers. J Natl Compr Canc Netw. 2017;15(1):46-55.
10. Huo J, Bian J, Xie Z, et al. Patterns of postdiagnosis depression among late-stage cancer patients: do racial/ethnic and sex disparities exist? Am J Clin Oncol. 2019;42(8):675-681.
11. Ashing-Giwa K, Rosales M, Lai L, et al. Depressive symptomatology among Latina breast cancer survivors. Psychooncology. 2013;22(4):845-853.
12. American Society of Clinical Oncology Clinical Practice Survivorship Guidelines and Adaptations: Summary of Recommendations Tables. 2014. https://www.asco.org/sites/new-www.asco.org/files/content-files/practice-and-guidelines/documents/ASCO-guidelines-summary-of-recommendations-tables.pdf. Accessed July 15, 2022.
13. National Cancer Institute. Depression (PDQ®) Health Professional Version. https://www.cancer.gov/about-cancer/coping/feelings/depression-hp-pdq#_98. Accessed July 15, 2022.
14. National Comprehensive Cancer Network. 2020 Distress during cancer care. https://www.nccn.org/patients/guidelines/content/PDF/distress-patient.pdf. Accessed July 15, 2022.
15. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2030, Cancer. Increase quality of life for cancer survivors (C-R01). https://health.gov/healthypeople/objectives-and-data/browse-objectives/cancer/increase-quality-life-cancer-survivors-c-r01. Accessed August 1, 2022.
16. Hopko DR, Funderburk JS, Shorey RC, et al. Behavioral activation and problem-solving therapy for depressed breast cancer patients: preliminary support for decreased suicidal ideation. Behav Modif. 2013;37(6):747-767.
17. Manigault AW, Ganz PA, Irwin MR, et al. Moderators of inflammation-related depression: a prospective study of breast cancer survivors. Transl Psychiatry. 2021;11(1):615.
18. Manigault AW, Kuhlman KR, Irwin MR, et al. Vulnerability to inflammation-related depressive symptoms: moderation by stress in women with breast cancer. Brain Behav Immun. 2021;94:71-78.
19. Wang YH, Li JQ, Shi JF, et al. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry. 2020;25(7):1487-1499.
20. Shim EJ, Lee JW, Cho J, et al. Association of depression and anxiety disorder with the risk of mortality in breast cancer: a national health insurance service study in Korea. Breast Cancer Res Treat. 2020;179(2):491-498.
21. Chen SJ, Chang CH, Chen KC, et al. Association between depressive disorders and risk of breast cancer recurrence after curative surgery. Medicine (Baltimore). 2016;95(33):e4547.
22. Yu S, Li W, Tang L, et al. Depression in breast cancer patients: immunopathogenesis and immunotherapy. Cancer Lett. 2022;536:215648.
23. Irwin MR, Olmstead R, Kruse J, et al. Association of interleukin-8 and risk of incident and recurrent depression in long-term breast cancer survivors. Brain Behav Immun. 2022;105:131-138.
24. Zhang AY, Ganocy SJ, Owusu C, et al. Associations among irritability, high-sensitivity C-reactive protein/interleukin-6, and depression in patients with early-stage breast cancer undergoing chemotherapy: a prospective study. J Acad Consult Liaison Psychiatry. 2022;63(3):260-267.
25. Ho HY, Chin-Hung Chen V, et al. Circulating cytokines as predictors of depression in patients with breast cancer. J Psychiatr Res. 2021;136:306-311.
26. Jehn CF, Flath B, Strux A, et al. Influence of age, performance status, cancer activity, and IL-6 on anxiety and depression in patients with metastatic breast cancer. Breast Cancer Res Treat. 2012;136(3):789-794.
27. Cvetković J, Ivanović Kovačevic S, Cvetkovic M, et al. Evaluation of the role of stress in patients with breast cancer and depression by paykel's life event and adaptive neuro-fuzzy approach. Brain Behav. 2020;10(4):e01570.
28. Castro-Figueroa EM, Acevedo KI, Peña-Vargas CI, et al. Depression, anxiety, and social environmental adversity as potential modulators of the immune tumor microenvironment in breast cancer patients. Med Sci (Basel). 2021;9(2):46.
29. Bandinelli LP, Levandowski ML, Grassi-Oliveira R. The childhood maltreatment influences on breast cancer patients: a second wave hit model hypothesis for distinct biological and behavioral response. Med Hypotheses. 2017;108:86-93.
30. Manigault AW, Kuhlman KR, Irwin MR, et al. Psychosocial resilience to inflammation-associated depression: a prospective study of breast-cancer survivors. Psychol Sci. 2022;33(8):1328-1339.
31. Vilardaga JCP, Fisher HM, Winger JG, et al. Pain, depressive symptoms, and self-efficacy for pain management: examination in African-American women with breast cancer. Support Care Cancer. 2022;30(8):6633-6640.
32. Huang Z, Zhao J, Ding K, et al Depression involved in self-reported prospective memory problems in survivors of breast cancer who have received chemotherapy. Medicine (Baltimore). 2019;98(16):e15301.
33. Hajj A, Hachem R, Khoury R, et al. Clinical and genetic factors associated with the breast cancer-related sleep disorders: the “CAGE-Sleep” study−a cross-sectional study. J Pain Symptom Manage. 2021;62(3):e46-e55.
34. Buscariollo DL, Cronin AM, Borstelmann NA, et al. Impact of pre-diagnosis depressive symptoms and health-related quality of life on treatment choice for ductal carcinoma in situ and stage I breast cancer in older women. Breast Cancer Res Treat. 2019;173(3):709-717.
35. Eskelinen M, Korhonen R, Selander T, et al. Beck Depression Inventory as a predictor of long-term outcome among patients admitted to the breast cancer diagnosis unit: a 25-year cohort study in Finland. Anticancer Res. 2017;37(2):819-824.
36. Sun HL, Dong XX, Cong YJ, et al. Depression and the risk of breast cancer: a meta-analysis of cohort studies. Asian Pac J Cancer Prev. 2015;16(8):3233-3239.
37. Killgore WDS, Cloonan SA, Taylor EC, et al. Mental health during the first weeks of the COVID-19 pandemic in the United States. Front Psychiatry. 2021;12:561898.
38. Turgeman I, Goshen-Lago T, Waldhorn I, et al. Psychosocial perspectives among cancer patients during the coronavirus disease 2019 (COVID-19) crisis: an observational longitudinal study. Cancer Rep (Hoboken). 2022;5(5):e1506.
39. Dilawari A, Rentscher KE, Zhai W, et al; Thinking and Living with Cancer Study. Medical care disruptions during the first six months of the COVID-19 pandemic: the experience of older breast cancer survivors. Breast Cancer Res Treat. 2021;190(2):287-293.
40. Mink van der Molen DR, Bargon CA, Batenburg MCT, et al; UMBRELLA study group. (Ex-)breast cancer patients with (pre-existing) symptoms of anxiety and/or depression experience higher barriers to contact health care providers during the COVID-19 pandemic. Breast Cancer Res Treat. 2021;186(2):577-583.
41. Bargon CA, Batenburg MCT, van Stam LE, et al. Impact of the COVID-19 pandemic on patient-reported outcomes of breast cancer patients and survivors. JNCI Cancer Spectr. 2020;5(1):pkaa104.
42. Rentscher KE, Zhou X, Small BJ, et al. Loneliness and mental health during the COVID-19 pandemic in older breast cancer survivors and noncancer controls. Cancer. 2021;127(19):3671-3679.
43. Yousefi Afrashteh M, Masoumi S. Psychological well-being and death anxiety among breast cancer survivors during the Covid-19 pandemic: the mediating role of self-compassion. BMC Womens Health. 2021;21(1):387.
44. Kállay É, Medrea F, Dégi CL. On top of that all, now Covid-19, too. A scoping review of specificities and correlates of fear of cancer recurrence in breast cancer patients during COVID-19. Breast. 2022;62:123-134.
45. He S, Wang Y, Zhao X, et al. Factors influencing delayed treatment in patients with breast cancer during COVID-19 pandemic. Front Public Health. 2022;10:808873.
46. Kim SY, Kim S. Do COVID-19-related treatment changes influence fear of cancer recurrence, anxiety, and depression in breast cancer patients? Cancer Nurs. 2022;45(2):E628-E638.
47. Budisavljevic A, Kelemenic-Drazin R, Dedic Plavetic N, et al. The first wave of the COVID-19 pandemic and its impact on the level of distress in patients with breast cancer, a multicentric study. Psychiatr Danub. 2021;33(Suppl 13):341-349.
48. Massicotte V, Ivers H, Savard J. COVID-19 pandemic stressors and psychological symptoms in breast cancer patients. Curr Oncol. 2021;28(1):294-300.
49. Chiesi F, Vizza D, Valente M, et al. Positive personal resources and psychological distress during the COVID-19 pandemic: resilience, optimism, hope, courage, trait mindfulness, and self-efficacy in breast cancer patients and survivors. Support Care Cancer. 2022;30(8):7005-7014.
50. Hulbert-Williams NJ, Leslie M, Hulbert-Williams L, et al. Evaluating the impact of COVID-19 on supportive care needs, psychological distress and quality of life in UK cancer survivors and their support network. Eur J Cancer Care (Engl). 2021;30(5):e13442.
51. Bartmann C, Fischer LM, Hübner T, et al. The effects of the COVID-19 pandemic on psychological stress in breast cancer patients. BMC Cancer. 2021;21(1):1356.
52. Bártolo A, Santos IM, Valério E, et al. Depression and health-related quality of life among young adult breast cancer patients: the mediating role of reproductive concerns. J Adolesc Young Adult Oncol. 2020;9(3):431-435.
53. Yfantis A, Intas G, Tolia M, et al. Health-related quality of life of young women with breast cancer. Review of the literature. J BUON. 2018;23(1):1-6.
54. Gorman JR, Malcarne VL, Roesch SC, et al. Depressive symptoms among young breast cancer survivors: the importance of reproductive concerns. Breast Cancer Res Treat. 2010;123(2):477-485.
55. Lee M, Kim YH, Jeon MJ. Risk factors for negative impacts on sexual activity and function in younger breast cancer survivors. Psychooncology. 2015;24(9):1097-1103.
56. Borstelmann NA, Rosenberg SM, Ruddy KJ, et al. Partner support and anxiety in young women with breast cancer. Psychooncology. 2015;24(12):1679-1685.
57. CDC. Breast cancer in young women. https://www.cdc.gov/cancer/breast/young_women/bringyourbrave/breast_cancer_young_women/index.htm#:~:text=Although%20breast%20cancer%20mostly%20occurs,than%2045%20years%20of%20age. Accessed July 15, 2022.
58. Howell DM, Metcalfe K, Kong S, et al. Risk factors for psychological morbidity and the protective role of coping self-efficacy in young women with breast cancer early in diagnosis: a national multicentre cohort study. Breast Cancer Res Treat. 2022;194(1):91-102.
59. Howard-Anderson J, Ganz PA, Bower JE, et al. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104(5):386-405.
60. Ganz PA, Bower JE, Partridge AH, et al. Screening for depression in younger breast cancer survivors: outcomes from use of the 9-item Patient Health Questionnaire. JNCI Cancer Spectr. 2021;5(3):pkab017.
61. Muzzatti B, Bomben F, Flaiban C, et al. Quality of life and psychological distress during cancer: a prospective observational study involving young breast cancer female patients. BMC Cancer. 2020;20(1):758.
62. Fernandes-Taylor S, Adesoye T, Bloom JR. Managing psychosocial issues faced by young women with breast cancer at the time of diagnosis and during active treatment. Curr Opin Support Palliat Care. 2015;9(3):279-284.
63. Park EM, Gelber S, Rosenberg SM, et al. Anxiety and depression in young women with metastatic breast cancer: a cross-sectional study. Psychosomatics. 2018;59(3):251-258.
64. American Cancer Society. Breast cancer facts and figures 2019-2020. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf. Accessed July 15, 2022.
65. National Cancer Institute. Fertility preservation safe for young women with breast cancer. December 2, 2020. https://www.cancer.gov/news-events/cancer-currents-blog/2020/breast-cancer-fertility-preservation-safe Accessed July 15, 2022.
66. Goldrat O, De Cooman M, Mailliez A, et al. Efficacy and safety of controlled ovarian hyperstimulation with or without letrozole for fertility preservation in breast cancer patients: a multicenter retrospective study. Eur J Cancer. 2022;174:134-141.
67. Marklund A, Lundberg FE, Eloranta S, et al. Reproductive outcomes after breast cancer in women with vs without fertility preservation. JAMA Oncol. 2021;7(1):86-91.
68. Marklund A, Lekberg T, Hedayati E, et al. Relapse rates and disease-specific mortality following procedures for fertility preservation at time of breast cancer diagnosis. JAMA Oncol. 2022 Aug 25;e223677.
69. Bártolo A, Neves M, Carvalho B, et al. Fertility under uncertainty: exploring differences in fertility-related concerns and psychosocial aspects between breast cancer survivors and non-cancer infertile women. Breast Cancer. 2020;27(6):1177-1186.
70. Greaney ML, Sprunck-Harrild K, Ruddy KJ, et al. Study protocol for Young & Strong: a cluster randomized design to increase attention to unique issues faced by young women with newly diagnosed breast cancer. BMC Public Health. 2015;15:37.
71. Partridge AH, Ruddy KJ, Barry WT, et al. A randomized study to improve care for young women with breast cancer at community and academic medical oncology practices in the United States: the Young and Strong study. Cancer. 2019;125(11):1799-1806.
72. Peate M, Meiser B, Cheah BC, et al. Making hard choices easier: a prospective, multicentre study to assess the efficacy of a fertility-related decision aid in young women with early-stage breast cancer. Br J Cancer. 2012;106(6):1053-1061.
73. Accortt EE, Bower JE, Stanton AL, et al. Depression and vasomotor symptoms in young breast cancer survivors: the mediating role of sleep disturbance. Arch Womens Ment Health. 2015;18(3):565-568.
74. Katapodi MC, Ellis KR, Schmidt F, et al. Predictors and interdependence of family support in a random sample of long-term young breast cancer survivors and their biological relatives. Cancer Med. 2018;7(10):4980-4992.
75. Baudry AS, Yakimova S, Congard A, et al. Adjustment of young women with breast cancer after chemotherapy: a mediation model of emotional competence via emotional distress. Psychooncology. 2022;31(5):848-855.
76. Cook EE, Rosenberg SM, Ruddy KJ, et al. Prospective evaluation of the impact of stress, anxiety, and depression on household income among young women with early breast cancer from the Young and Strong trial. BMC Public Health. 2020;20(1):1514.
77. Rosenberg SM, Tamimi RM, Gelber S, et al. Body image in recently diagnosed young women with early breast cancer. Psychooncology. 2013;22(8):1849-1855.
78. Rosenberg SM, Dominici LS, Gelber S, et al. Association of breast cancer surgery with quality of life and psychosocial well-being in young breast cancer survivors. JAMA Surg. 2020;155(11):1035-1042.
79. Bower JE, Partridge AH, Wolff AC, et al. Targeting depressive symptoms in younger breast cancer survivors: the Pathways to Wellness randomized controlled trial of mindfulness meditation and survivorship education. J Clin Oncol. 2021;39(31):3473-3484.
80. Di Giacomo D, Ranieri J, Guerra F, et al. Survivorship in young women after early breast cancer: a cross-sectional study of emotional traits along 3-years perspective. Riv Psichiatr. 2019;54(4):160-167.
81. Ventura EE, Ganz PA, Bower JE, et al. Barriers to physical activity and healthy eating in young breast cancer survivors: modifiable risk factors and associations with body mass index. Breast Cancer Res Treat. 2013;142(2):423-433.
82. Borstelmann NA, Rosenberg S, Gelber S, et al. Partners of young breast cancer survivors: a cross-sectional evaluation of psychosocial concerns, coping, and mental health. J Psychosoc Oncol. 2020;38(6):670-686.
83. Duprez C, Vanlemmens L, Untas A, et al. Emotional distress and subjective impact of the disease in young women with breast cancer and their spouses. Future Oncol. 2017;13(29):2667-2680.
84. Soltamox (tamoxifen citrate oral solution) prescribing information. Raleigh, NC: Midatech Pharma; September 2018.
85. Stäuble CK, Lampert ML, Allemann S, et al. Pharmacist-guided pre-emptive pharmacogenetic testing in antidepressant therapy (PrePGx): study protocol for an open-label, randomized controlled trial. Trials. 2021;22(1):919.
86. Argalácsová S, Slanař O, Vítek P, et al. Contribution of ABCB1 and CYP2D6 genotypes to the outcome of tamoxifen adjuvant treatment in premenopausal women with breast cancer. Physiol Res. 2015;64(suppl 4):S539-S547.
87. Wang T, Zhou Y, Cao G. Pharmacogenetics of tamoxifen therapy in Asian populations: from genetic polymorphism to clinical outcomes. Eur J Clin Pharmacol. 2021;77(8):1095-1111.
88. Tulsyan S, Mittal RD, Mittal B. The effect of ABCB1 polymorphisms on the outcome of breast cancer treatment. Pharmgenomics Pers Med. 2016;9:47-58.
89. Argalacsova S, Slanar O, Bakhouche H, et al. Impact of ABCB1 and CYP2D6 polymorphisms on tamoxifen treatment outcomes and adverse events in breast cancer patients. J BUON. 2017;22(5):1217-1226.
90. Clinical Pharmacogenetics Implementation Consortium (CPIC). CPIC guideline for tamoxifen based on CYP2D6 genotype. https://cpicpgx.org/guidelines/cpic-guideline-for-tamoxifen-based-on-cyp2d6-genotype/. Accessed July 15, 2022.
91. Goetz MP, Sangkuhl K, Guchelaar HJ, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for CYP2D6 and tamoxifen therapy. Clin Pharmacol Ther. 2018;103(5):770-777.
92. Drugs.com. Tamoxifen. https://www.drugs.com/monograph/tamoxifen.html. Accessed August 1, 2022.
93. Cronin-Fenton D, Lash TL, Sørensen HT. Selective serotonin reuptake inhibitors and adjuvant tamoxifen therapy: risk of breast cancer recurrence and mortality. Future Oncol. 2010;6(6):877-880.
94. Lyon E, Gastier Foster J, Palomaki GE, et al; working group of the Molecular Genetics Subcommittee on behalf of the American College of Medical Genetics and Genomics (ACMG) Laboratory Quality Assurance Committee. Laboratory testing of CYP2D6 alleles in relation to tamoxifen therapy. Genet Med. 2012;14(12):990-1000.
95. Lum DW, Perel P, Hingorani AD, et al. CYP2D6 genotype and tamoxifen response for breast cancer: a systematic review and meta-analysis. PLoS One. 2013;8(10):e76648.
96. Bradbury M, Hutton B, Beltran-Bless AA, et al. Time to update evidence-based guideline recommendations about concurrent tamoxifen and antidepressant use? A systematic review. Clin Breast Cancer. 2022;22(3):e362-e373.
97. Dusetzina SB, Alexander GC, Freedman RA, et al. Trends in co-prescribing of antidepressants and tamoxifen among women with breast cancer, 2004-2010. Breast Cancer Res Treat. 2013;137(1):285-296.
98. Dieudonné AS, De Nys K, Casteels M, et al. How often did Belgian physicians co-prescribe tamoxifen with strong CYP2D6 inhibitors over the last 6 years? Acta Clin Belg. 2014;69(1):47-52.
99. FDA. Drug development and drug interactions--table of substrates, inhibitors, and inducers. https://www.fda.gov/drugs/drug-interactions-labeling/drug-development-and-drug-interactions-table-substrates-inhibitors-and-inducers#table2-2. Accessed July 15, 2022.
100. McMichael KS, Adams K, Breden Crouse EL. Tamoxifen and depression: drug interactions in breast cancer. Consult Pharm. 2013;28(9):584-591.
101. Hicks JK, Bishop JR, Sangkuhl K, et al; Clinical Pharmacogenetics Implementation Consortium. Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for CYP2D6 and CYP2C19 genotypes and dosing of selective serotonin reuptake inhibitors. Clin Pharmacol Ther. 2015;98(2):127-134.
102. FDA. Table of pharmacogenetic associations. https://www.fda.gov/medical-devices/precision-medicine/table-pharmacogenetic-associations. Accessed July 15, 2022.
103. Stearns V, Johnson MD, Rae JM, et al. Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J Natl Cancer Inst. 2003;95(23):1758-1764.
104. Jin Y, Desta Z, Stearns V, et al. CYP2D6 genotype, antidepressant use, and tamoxifen metabolism during adjuvant breast cancer treatment. J Natl Cancer Inst. 2005;97(1):30-39.
105. Lash TL, Pedersen L, Cronin-Fenton D, et al. Tamoxifen’s protection against breast cancer recurrence is not reduced by concurrent use of the SSRI citalopram. Br J Cancer. 2008;99(4):616-621.
106. Lash TL, Cronin-Fenton D, Ahern TP, et al. Breast cancer recurrence risk related to concurrent use of SSRI antidepressants and tamoxifen. Acta Oncol. 2010;49(3):305-312.
107. Kelly CM, Juurlink DN, Gomes T, et al. Selective serotonin reuptake inhibitors and breast cancer mortality in women receiving tamoxifen: a population based cohort study. BMJ. 2010;340:c693.
108. Haque R, Shi J, Schottinger JE, et al. Tamoxifen and antidepressant drug interaction in a cohort of 16,887 breast cancer survivors. J Natl Cancer Inst. 2015;108(3):djv337.
109. Valachis A, Garmo H, Weinman J, et al. Effect of selective serotonin reuptake inhibitors use on endocrine therapy adherence and breast cancer mortality: a population-based study. Breast Cancer Res Treat. 2016;159(2):293-303.
110. Boursi B, Lurie I, Haynes K, et al. Chronic therapy with selective serotonin reuptake inhibitors and survival in newly diagnosed cancer patients. Eur J Cancer Care (Engl). 2018;27(1).
111. Chubak J, Bowles EJ, Yu O, et al. Breast cancer recurrence in relation to antidepressant use. Cancer Causes Control. 2016;27(1):125-136.
112. Federalregister.gov. Clinical Pharmacology Subcommittee of the Advisory Committee for Pharmaceutical Science; Notice of Meeting. Fed Reg. August 29, 2006;71(167): 51198. https://www.federalregister.gov/documents/2006/08/29/E6-14296/clinical-pharmacology-subcommittee-of-the-advisory-committee-for-pharmaceutical-science-notice-of. Accessed July 15, 2022.
113. Henry NL, Stearns V, Flockhart DA, et al. Drug interactions and pharmacogenomics in the treatment of breast cancer and depression. Am J Psychiatry. 2008;165(10):1251-1255.
114. LLerena A, Naranjo MEG, Rodrigues-Soares F, et al. Interethnic variability of CYP2D6 alleles and of predicted and measured metabolic phenotypes across world populations. Expert Opin Drug Metab Toxicol. 2014;10(11):1569-1583.
115. Ting S, Schug S. The pharmacogenomics of pain management: prospects for personalized medicine. J Pain Res. 2016;9:49-56.
116. Gaedigk A, Sangkuhl K, Whirl-Carrillo M, et al. Prediction of CYP2D6 phenotype from genotype across world populations. Genet Med. 2017;19(1):69-76.
117. Papastergiou J, Quilty LC, Li W, et al. Pharmacogenomics guided versus standard antidepressant treatment in a community pharmacy setting: a randomized controlled trial. Clin Transl Sci. 2021;14(4):1359-1368.
118. Desmarais JE, Looper KJ. Managing menopausal symptoms and depression in tamoxifen users: implications of drug and medicinal interactions. Maturitas. 2010;67(4):296-308.
119. Nichols AI, Lubaczewski S, Liang Y, et al. Open-label, 2-period sequential drug interaction study to evaluate the effect of a 100-mg dose of desvenlafaxine on the pharmacokinetics of tamoxifen when coadministered in healthy postmenopausal female subjects. Int J Clin Pharmacol Ther. 2014;52(10):830-841.
120. Binkhorst L, Bannink M, de Bruijn P, et al. Augmentation of endoxifen exposure in tamoxifen-treated women following SSRI switch. Clin Pharmacokinet. 2016;55(2):249-255.
121. Hussaarts KGAM, Berger FA, Binkhorst L, et al. The risk of QTc-interval prolongation in breast cancer patients treated with tamoxifen in combination with serotonin reuptake inhibitors. Pharm Res. 2019;37(1):7.
122. Juurlink D. Revisiting the drug interaction between tamoxifen and SSRI antidepressants. BMJ. 2016;354:i5309.
123. Drugs.com. Interaction between tamoxifen and St. John’s wort. https://www.drugs.com/interactions-check.php?drug_list=2145-0,2106-0&types%5B%5D=major&types%5B%5D=minor&types%5B%5D=moderate&types%5B%5D=food&types%5B%5D=therapeutic_duplication&professional=1. Accessed July 15, 2022.
124. Bourque F, Karama S, Looper K, et al. Acute tamoxifen-induced depression and its prevention with venlafaxine. Psychosomatics. 2009;50(2):162-165.
125. Gaitanidis A, Alevizakos M, Pitiakoudis M, et al. Trends in incidence and associated risk factors of suicide mortality among breast cancer patients. Psychooncology. 2018;27(5):1450-1456.
126. Twombly R. Decades after cancer, suicide risk remains high. J Natl Cancer Inst. 2006;98(19):1356-1358.
127. Güth U, Myrick ME, Reisch T, et al. Suicide in breast cancer patients: an individual-centered approach provides insight beyond epidemiology. Acta Oncol. 2011;50(7):1037-1044.
128. Saad AM, Gad MM, Al-Husseini MJ, et al. Suicidal death within a year of a cancer diagnosis: a population-based study. Cancer. 2019;125(6):972-979.
129. Schairer C, Brown LM, Chen BE, et al. Suicide after breast cancer: an international population-based study of 723,810 women. J Natl Cancer Inst. 2006;98(19):1416-1419.
130. Kim JM, Jang JE, Stewart R, et al. Determinants of suicidal ideation in patients with breast cancer. Psychooncology. 2013;22(12):2848-2856.
131. Kim JM, Kang HJ, Kim SY, et al. BDNF promoter methylation associated with suicidal ideation in patients with breast cancer. Int J Psychiatry Med. 2015;49(1):75-94.
132. Kazlauskiene J, Navickas A, Lesinskiene S, et al. Factors affecting suicidal thoughts in breast cancer patients. Medicina (Kaunas). 2022;58(7):863.
133. Matsumoto Y, Shimizu K, Kinoshita H, et al. Suicide associated with corticosteroid use during chemotherapy: case report. Jpn J Clin Oncol. 2010;40(2):174-176.
134. Le GM, O’Malley CD, Glaser SL, et al. Breast implants following mastectomy in women with early-stage breast cancer: prevalence and impact on survival. Breast Cancer Res. 2005;7(2):R184-R193.
135. Brinton LA. Do breast implants after a mastectomy affect subsequent prognosis and survival? Breast Cancer Res. 2005;7(2):61-63.
136. Eskelinen M, Korhonen R, Selander T, et al. Suicidal ideation versus hopelessness/helplessness in healthy individuals and in patients with benign breast disease and breast cancer: a prospective case-control study in Finland. Anticancer Res. 2015;35(6):3543-3551.
137. Suicide Prevention Resource Center. Problem-solving therapy (PST). https://sprc.org/resources-programs/problem-solving-therapy-pst. Accessed August 12, 2022.
138. Suppli NP, Johansen C, Kessing LV, et al. Survival after early-stage breast cancer of women previously treated for depression: a nationwide Danish cohort study. J Clin Oncol. 2017;35(3):334-342.
139. Congress.gov. S.2661 - National Suicide Hotline Designation Act of 2020. https://www.congress.gov/bill/116th-congress/senate-bill/2661 Accessed August 12, 2022.
140. Federal Communications Commission. 988 suicide & crisis lifeline fact sheet. https://www.fcc.gov/sites/default/files/988-fact-sheet.pdf. Accessed August 12, 2022.
141. Well Being Trust. Consensus approach and recommendations for the creation of a comprehensive crisis response system. https://www.datocms-assets.com/12810/1637261286-988-crisis-response-report-november-final.pdf. Accessed August 12, 2022.
142. Substance Abuse and Mental Health Services Administration (SAMHSA). 988 suicide & crisis lifeline fact sheet. https://www.samhsa.gov/sites/default/files/988-factsheet.pdf. Accessed August 12, 2022.
143. O’Reilly CL, Wong E, Chen TF. A feasibility study of community pharmacists performing depression screening services. Res Social Adm Pharm. 2015;11(3):364-381.
144. Denson BH, Kim RE. Evaluation of provider response to positive depression screenings and physician attitudes on integrating psychiatric pharmacist services in primary care settings. Ment Health Clin. 2018;8(1):28-32.
145. Rosser S, Frede S, Conrad WF, Heaton PC. Development, implementation, and evaluation of a pharmacist-conducted screening program for depression. J Am Pharm Assoc (2003). 2013;53(1):22-29.
146. Hare SK, Kraenow K. Depression screenings: developing a model for use in a community pharmacy. J Am Pharm Assoc (2003). 2008;48(1):46-51.
147. Ito T, Shimizu K, Ichida Y, et al. Usefulness of pharmacist-assisted screening and psychiatric referral program for outpatients with cancer undergoing chemotherapy. Psychooncology. 2011;20(6):647-654.
148. Knight DE, Draeger RW, Heaton PC, et al. Pharmacist screening for depression among patients with diabetes in an urban primary care setting. J Am Pharm Assoc (2003). 2008;48(4):518-521.
149. Wilson C, Twigg G. Pharmacist-led depression screening and intervention in an underserved, rural, and multi-ethnic diabetic population. J Am Pharm Assoc (2003). 2018;58(2):205-209.
150. Zmoira A, Rogers E, Johnson A, et al. Implementation of a depression screening as part of a holistic adherence assessment in a large community pharmacy chain. J Am Pharm Assoc (2003). 2021;61(4S):S154-S160.
151. Wells BG. Underrecognition and undertreatment of depression: what is the pharmacist’s culpability? Pharmacotherapy. 1999;19(11):1237-1239.
152. Ragland D, Payakachat N, Hays EB, et al. Depression and diabetes: establishing the pharmacist’s role in detecting comorbidity in pregnant women. J Am Pharm Assoc (2003). 2010;50(2):195-199.
153. Elkhodr S, Saba M, O’Reilly C, et al. The role of community pharmacists in the identification and ongoing management of women at risk for perinatal depression: a qualitative study. Int J Soc Psychiatry. 2018;64(1):37-48.
154. Cohen LB, Taveira TH, Wu WC, et al. Pharmacist-led telehealth disease management program for patients with diabetes and depression. J Telemed Telecare. 2020;26(5):294-302.
155. Readdean KC, Heuer AJ, Scott Parrott J. Effect of pharmacist intervention on improving antidepressant medication adherence and depression symptomology: a systematic review and meta-analysis. Res Social Adm Pharm. 2018;14(4):321-331.
156. Stuhec M, Zelko E. A collaborative care model between general practitioners and clinical pharmacists in a community health centre setting in depression treatment. Psychiatr Danub. 2021;33(suppl 4):1261-1266.
157. Mospan CM, Gillette C, McKee J, et al. Community pharmacists as partners in reducing suicide risk. J Am Board Fam Med. 2019;32(6):763-767.
158. Rickles NM. Filling a global gap in access to critical mental health services: engaging pharmacists to enhance the care of individuals with mental health needs and illnesses. J Am Pharm Assoc (2003). 2020;60(5S):S5-S6.
159. Mospan CM, Gillette C, Wilson JA. Patient and prescriber perceptions of depression screening within a community pharmacy setting. J Am Pharm Assoc (2003). 2020;60(5S):S15-S22.
160. APhA Foundation. White paper on expanding the role of the community pharmacist in managing depression. https://www.aphafoundation.org/sites/default/files/ckeditor/files/WhitePaper-PharmacistRoleManagingDepression-APhAFoundation-2009(1).pdf. Accessed July 15, 2022.
161. American Society of Health-System Pharmacists. Policy positions. 1901: Suicide awareness and prevention. https://www.ashp.org/-/media/assets/policy-guidelines/docs/policy-positions/policy-positions-specific-practice-areas.pdf. Accessed July 15, 2022.
162. Morden E, Byron S, Roth L, et al. Health plans struggle to report on depression quality measures that require clinical data. Acad Pediatr. 2022;22(3S):S133-S139.
163. Centers for Medicare and Medicaid Services (CMS). Health Insurance Exchange. 2023 Quality rating system measure technical specifications. March 2022. https://www.cms.gov/files/document/2023-qrs-technical-specifications.pdf. Accessed September 24, 2022.
164. Mental Health First Aid. www.mentalhealthfirstaid.org. Accessed July 15, 2022.
165. O’Reilly CL, Bell JS, Kelly PJ, et al. Impact of mental health first aid training on pharmacy students’ knowledge, attitudes and self-reported behaviour: a controlled trial. Aust N Z J Psychiatry. 2011;45(7):549-557.
166. Dollar KJ, Ruisinger JF, Graham EE, et al. Public awareness of Mental Health First Aid and perception of community pharmacists as Mental Health First Aid providers. J Am Pharm Assoc (2003). 2020;60(5S):S93-S97.e1.
167. Board of Pharmacy Specialties. Psychiatric pharmacy. https://www.bpsweb.org/bps-specialties/psychiatric-pharmacy/. Accessed August 31, 2022.
168. Finley PR, Bluml BM, Bunting BA, et al. Clinical and economic outcomes of a pilot project examining pharmacist-focused collaborative care treatment for depression. J Am Pharm Assoc (2003). 2011;51(1):40-49.
169. Silvia R, Plum M, Dufresne R. Efficiencies and outcomes of depression treatment by a psychiatric pharmacist in a primary care clinic compared with treatment within a behavioral health clinic. J Am Pharm Assoc (2003). 2020;60(5S):S98-S106.
170. Winchester BR, Watkins SC, Brahm NC, et al. Mental health treatment associated with community-based depression screening: considerations for planning multidisciplinary collaborative care. Ann Pharmacother. 2013;47(6):797-804.
171. Adler DA, Bungay KM, Wilson IB, et al. The impact of a pharmacist intervention on 6-month outcomes in depressed primary care patients. Gen Hosp Psychiatry. 2004;26(3):199-209.
172. Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37-49.
173. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361-370.
174. Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12(2):277-287.
175. Saracino RM, Weinberger MI, Roth AJ, et al. Assessing depression in a geriatric cancer population. Psychooncology. 2017;26(10):1484-1490.
176. Miller P, Newby D, Walkom E, et al. Depression screening in adults by pharmacists in the community: a systematic review. Int J Pharm Pract. 2020;28(5):428-440.